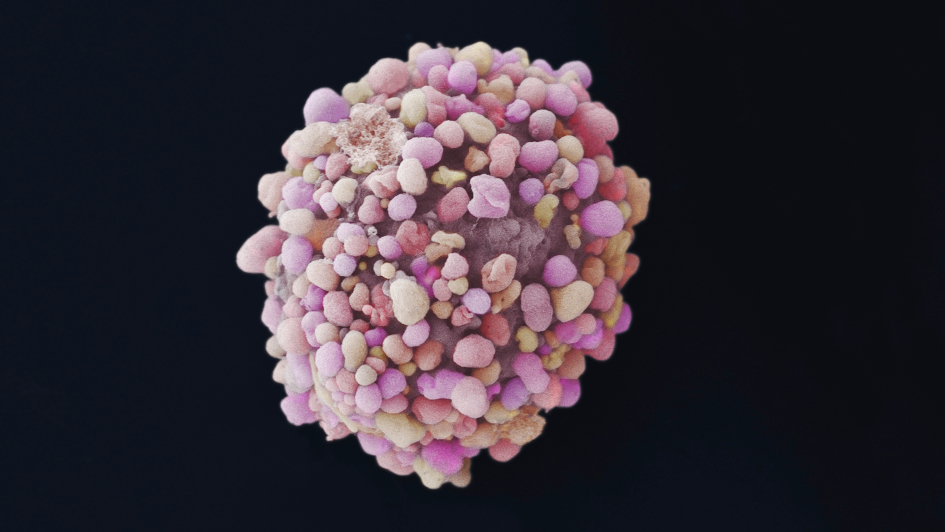
Image: Breast cancer cell. Image credit: Anne Weston, Francis Crick Institute. Licence: CC-BY-NC-4.0.
Scientists in our Division for Breast Cancer Research have been involved in some of the most famous discoveries in the history of breast cancer research.
They discovered the BRCA2 gene, for example, and over the past 20 years have been pioneers in establishing the concept of ‘synthetic lethality’ in cancer research and treatment. Their work underpinned and stimulated the development of olaparib and other PARP inhibitors – now standard treatments for genetic breast and platinum-sensitive ovarian cancers.
In the past five years, results of a clinical trial co-led by Professor Andrew Tutt, Head of our Division of Breast Cancer, have also established carboplatin – a drug discovered at the ICR – as a better treatment for BRCA1 and BRCA2 mutated forms of advanced breast cancer than the usual breast cancer standard.
Many of our successes in breast cancer research have come from The Breast Cancer Now Toby Robins Research Centre at the ICR.
The integrated teams at the ICR, together with colleagues at our partner hospital The Royal Marsden NHS Foundation Trust and through Breast Cancer Now programme integration with King’s College London and Guy’s Cancer Centre at Guy’s and St Thomas’ NHS Foundation Trust, have committed to define what they term ‘the evolving unmet need for breast cancer research’ by 2025 – with funding from Breast Cancer Now underpinning these ambitious plans.
The Division of Breast Cancer Research, which incorporates the Breast Cancer Now Research Centre, contains over 100 scientists and clinicians working in 12 teams.
Demonstrating impact
Researchers at the Centre lead important programmes to understand the genetic and environmental causes of breast cancer, and how a tumour’s molecular biology and surrounding microenvironment affect its behaviour and response to treatment.
They are also working on identifying new therapeutic approaches to breast cancer, and understanding the mechanisms tumours use in becoming resistant to treatment.
In a recent review of the Centre’s funding by Breast Cancer Now, Professor Tutt and colleagues across the centre set out a raft of successes over the past five years – including 398 research manuscripts, two new drug discovery programmes, the development of a new drug candidate, and 13 breast cancer clinical trials.
The Centre is clear in its aims to keep the fundamental science taking place in its laboratories relevant to real patient problems. This includes close collaboration with hospital colleagues, a focus on rarer but biologically distinct forms of breast cancers, the study of tumour evolution during treatment in clinical trials, and extending the impact of findings to broader patient groups.
Changing clinical practice
First, a thank you to Professor Mitch Dowsett, Head of the joint Academic Department of Biochemistry at The Royal Marsden and the ICR. Professor Dowsett’s work on the role of hormones in breast cancer has led to the development of both the most effective endocrine therapy treatments used for patients today – and the biomarkers that identify those who may benefit most from them – helping patients to avoid lengthy treatments and chemotherapy. Professor Dowsett's work on endocrine therapy resistance has been led with Dr Lesley-Ann Martin.
This work will sadly not be continuing in the next five-year round of funding from Breast Cancer Now as Professor Dowsett scales down his work. We are hugely proud of the team's myriad achievements to date, and the centre will continue research into hormones and breast cancer with Professor Stephen Johnston at The Royal Marsden and new appointments to ICR Faculty including Professor Cathrin Brisken.
The approval of the innovative breast cancer drug palbociclib is another example of the Centre’s success in achieving meaningful improvements for patients in the past five years.
Palbociclib is known as a first-in-class drug, because it’s the first drug to work in the way that it does – blocking two proteins, called CDK4 and CDK6 that help cancer cells divide and spread.
Professor Nicholas Turner, Professor in Molecular Oncology at the ICR and Consultant Oncologist at The Royal Marsden led a key clinical trial of palbociclib, showing that it could slow the progression of advanced breast cancer in conjunction with standard treatments, and substantially extend the lives of patients.
This innovation is already changing lives – more than 90,000 patients have been prescribed the drug.
Professor Turner, along with Professor Spiros Linardopoulos, Head of Drug Discovery at the Centre and other colleagues, continue to work on how resistance develops and how it may be targeted.
ICR patient advocate Christine was initially diagnosed with breast cancer in 2012 but, nearly five years after surgery and chemotherapy left her seemingly cancer free, she found the disease had returned, and spread to her brain and bones.
Following radiotherapy, she needed a targeted treatment to keep her cancer at bay. Fortunately, palbociclib had been approved for use on the NHS just months before, thanks to clinical trials that showed how palbociclib could benefit patients.
Christine is doing well on palbociclib: “I’m on the 21st cycle and my cancer is currently stable,” she says. “I’m able to work part-time, and I can keep up my cycling, which would have been more difficult on conventional therapy.”
Bringing new drugs to the clinic
Professor Linardopoulos leads the Centre’s work to search for gene targets for which new anticancer drugs can be developed.
A recent success for his team helped to progress work on a new drug candidate effective against fast-dividing cells, including triple-negative breast cancers. The target for the drug is a protein known to play a key part in controlling cell division – monopolar spindle 1 (MSP1). The first clinical trial of the new treatment is under way at The Royal Marsden and will shortly expand to other NHS Hospital partners like Guy’s Hospital.
Professor Spiros Linardopoulos said: “This exciting cancer treatment uses cancer's rapid growth against it, by forcing cells through cell division so quickly that they accumulate fatal errors.
“With the drug now entering clinical trials, we can see how our translational approach at the ICR to get drugs from the lab to the clinic really has an impact for patients.”
Homing in on the niche, harder problems
Professor Tutt explains that: “together with other Team Leaders in the Breast Cancer Now centre at the ICR, there is a focus on driving progress to address niche, harder problems – which are biologically distinctive but often not an initial focus for industry.”
These are some examples of programmes of work currently taking place across the centre:
Unpicking the functional genetics of breast cancer risk
Dr Olivia Fletcher, Team Leader in Functional Genetic Epidemiology leads a team of genetic epidemiologists and molecular biologists working in partnership with the Breast Cancer Now Generations Study, the British Breast Cancer Study and other population-based studies.
Population based studies allow us important insights into who genetic variants are associated with breast cancer risk – specifically, variants that map to non-coding DNA, and which are as a result difficult to identify. Olivia’s team are understanding how some of these variants act to drive risks in the hope of identify groups for early detection or prevention strategies.
Targeting neighbouring healthy cells
Professor Clare Isacke, Team Leader in Molecular Cell Biology, is leading work to identify the processes by which tumour cells recruit and activate non-cancerous cells during metastasis, the process of cancer’s growth and spread from its original site.
The team is identifying strategies to effectively target these neighbouring heathy cells, due to the important part they play in modulating the response of tumour cells to treatment – and as a result, tumour progression and resistance.
Mobilising the body’s immune system
Mobilising the body’s immune system after cell death is one major area of focus and innovation for the centre. Professor Pascal Meier, Team Leader in Cell Death and Immunity, is leading a team to explore the complex relationship between cell death, immunity and tumour growth and survival.
In particular, the team is focussing on the role of cell death and inflammation in adaptation to tissue stress, treatment resistance and tumour surveillance.
The team hope that new combination treatments they are trialling will allow doctors to manipulate the types of cell death which occur after treatment with current standard-of-care drugs and emerging targeted therapies, to more effectively mobilise the body’s natural immune response and enable better treatment outcomes.
Exploiting vulnerabilities in different subsets of breast cancer
Biomarkers are biological products – like proteins or genes – that can be measured in patient samples to detect disease. Biomarker development plays an important role in allowing researchers the ability to identify different tumour subsets with great accuracy, and in turn – with a greater understanding of these subtypes – for the biomarkers to help predict disease outcome.
Dr Rachael Natrajan, Team Leader in Functional Genomics, is researching the ways in which different subtypes of breast cancer can be characterised through genetic analysis of the tumour, to understand how different subgroups of a cancer and subpopulations of cells or “clones” become treatment resistant and can cooperate in doing so to drive relapse.
Other teams are leading work to understand the different dependencies and potential new drug targets within different subpopulations of a tumour.
Professor Chris Lord, Deputy Head of the Division of Breast Cancer Research, approaches this as an expert in the field of synthetic lethality. The term refers to when scientists exploit the fatal effects of disruption of the activity of two genes even though either disruption alone would not be fatal for the cells. Combining the effect of mutations in the tumour and use of targeted drugs can allow potent and tumour specific therapeutic effects. His team use tumour cell models and CRISPR-CAS9 gene perturbation techniques to help build their understanding of models of resistance in tumour cells.
Professor Tutt and Professor Lord’s laboratories are also working together to understand and target DNA repair deficient and genetically unstable breast cancers. Professor Tutt’s group have a special focus on basal-like Triple Negative breast cancers and create tumour organoid models, using tumours from patients treated with drugs that target DNA damage response and DNA replication stress.
To date, breast cancer research at the ICR has had a huge impact in helping patients assess their risks of developing breast cancer, choose the right treatment options and live longer.
Bringing it all back to the clinic
Ultimately, the end-goal for everything taking place in our Division of Breast Cancer Research is to improve the outcome and quality of life of women with or at risk of breast cancer.
Professors Tutt and Turner, as practicing oncologists and trial leaders, work with many others in the Centre to translate findings through to clinical trials using an integrated and patient-focussed strategic approach.
The centre also works closely with the wider national Breast Cancer Now network of research centres, and the international breast cancer research community. In partnership with The Royal Marsden, the Centre acts as a beacon for discovering therapy approaches and developing proof of concept ‘early phase’ and international practice changing ‘late phase’ trials.
October is Breast Cancer Awareness Month – a good time to reflect on the Centre’s work ahead, as 2020 draws close and the next five-year phase for the Centre’s strategy begin in earnest. We know the work is in good hands.
