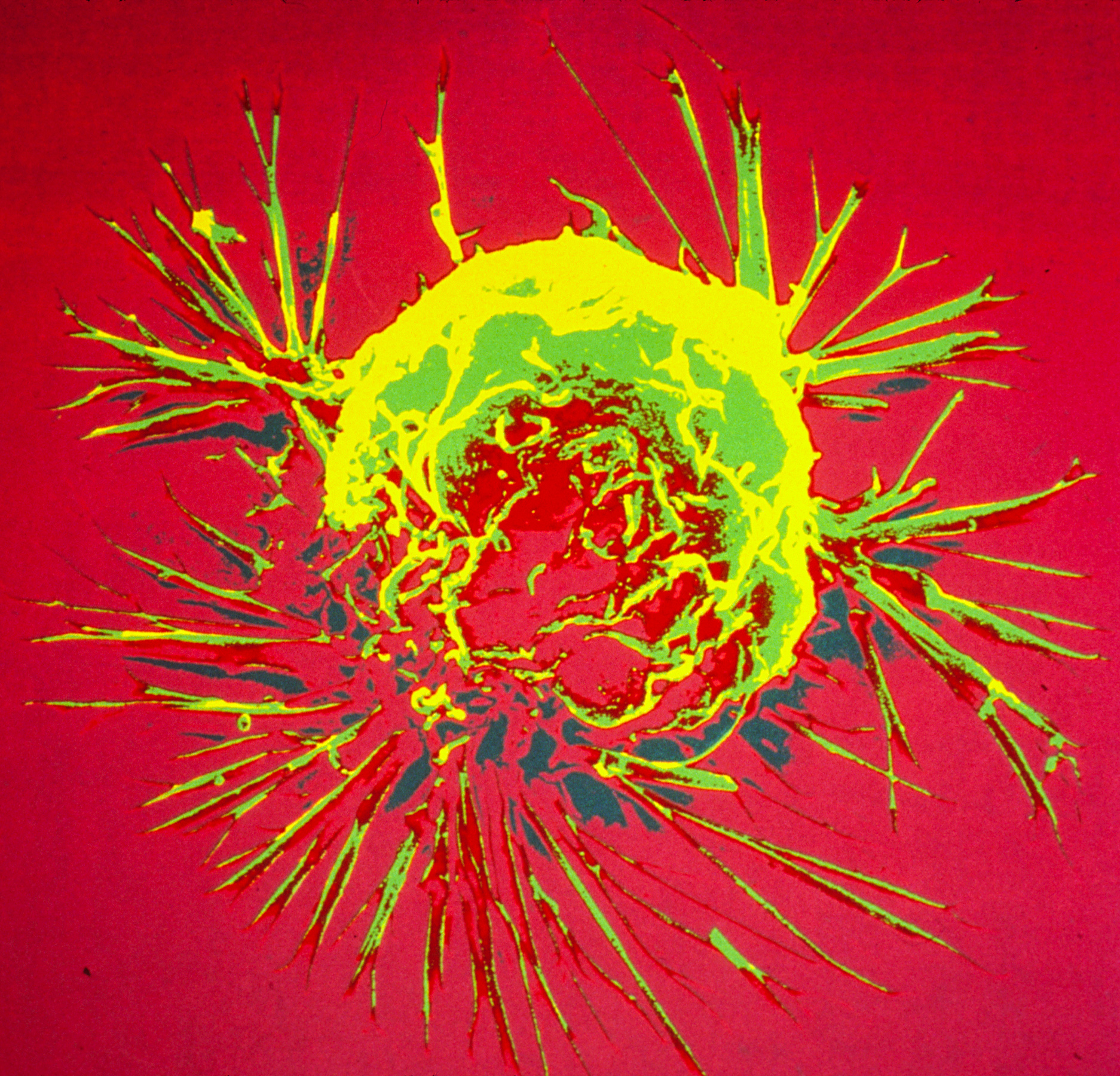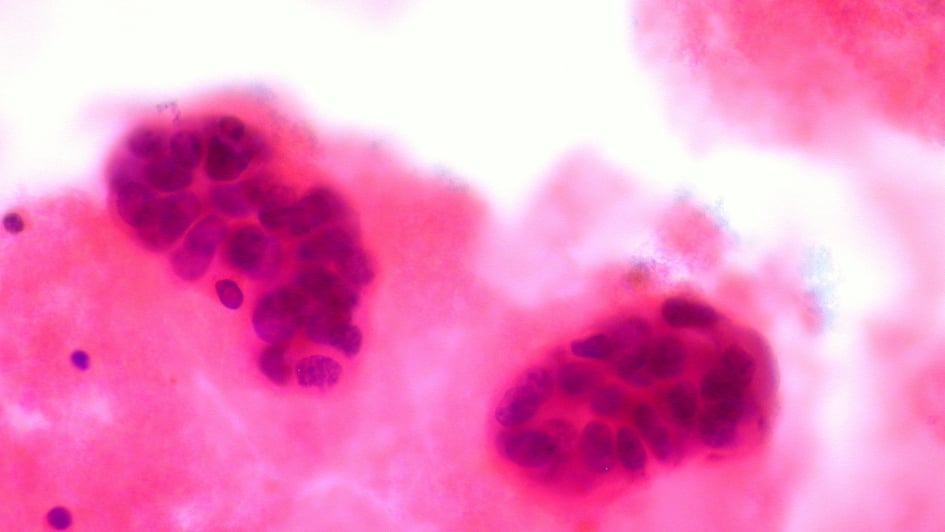
Image: Metastatic breast cancer in pleural fluid. Credit: Ed Uthman, Flickr with CC BY 2.0 license.
Adding a new targeted therapy to hormone therapy halts the growth of tumour cells in women with early-stage breast cancer, new research shows.
Giving women palbociclib – already hailed as a major step forward in treating advanced breast cancer – alongside hormone therapy had a much greater effect on cell growth than the hormone treatment alone.
Palbociclib alongside an aromatase inhibitor – a type of hormone treatment – shrank tumours in half of women with early-stage disease, a similar proportion to women who took the hormone therapy alone. But the drug combination led to a marked decrease in cell growth, stopping tumour growth entirely in 90 per cent of women, compared with 59 per cent given hormone therapy alone.
The large international trial was led by a team at The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust, in collaboration with researchers in the US. It was funded by the drug’s manufacturer, Pfizer.
Longer-term clinical trials are ongoing to assess if giving palbociclib alongside hormone therapy after surgery can delay breast cancer coming back.
The results were presented at the San Antonio Breast Cancer Symposium in Texas, and published in the Journal of Clinical Oncology today (Thursday).
See all of our most recent breast cancer related research news stories.
Palbociclib slowed growth and death of cancer cells
Hormone therapy is an effective treatment for hormone receptor-positive breast cancer, but the disease can return when tumours evolve to become resistant to treatment.
Combining hormone treatment with a targeted therapy such as palbociclib is one way of combating drug resistance – just as combination treatment is also used in diseases such as tuberculosis and HIV.
The trial was set up to test the benefit of adding palbociclib to treatment with an aromatase inhibitor before the patient had surgery – and to track the biological response to treatment for each patient.
The study involved 307 postmenopausal women with hormone receptor-positive breast cancer that had not begun to spread, and who had not yet had surgery to remove their tumour.
Researchers analysed tumour samples taken before, during and after a 14-week course of treatment – in order to analyse in detail the effect of the drug combination on the cancer’s biology and cell growth.
Patients received either the aromatase inhibitor, letrozole, or one of three different treatment schedules with a combination of letrozole and palbociclib.
Looking in closer detail at tumour samples from patients on the trial, the researchers found that adding palbociclib slowed both growth and death of cancer cells, explaining why tumours didn’t shrink as much as they had anticipated.
Healthy cells are programmed to die after a certain number of divisions or when something goes wrong – but cancer cells can avoid programmed cell death.
Patient benefit with palbociclib addition
Chief Investigator Professor Stephen Johnston, Consultant Medical Oncologist at The Royal Marsden, and Professor of Breast Cancer Medicine at The Institute of Cancer Research, London, said:
“Patients with breast cancer often respond to various drug treatments, only for the cancer cells to adapt, change or sidestep the initial beneficial effects. We have demonstrated that the current standard of care for many women – hormone treatment – is effective at stopping the growth of tumour cells prior to surgery, however with the addition of this new drug palbociclib patients may benefit even further.
“We are hopeful, based on the results of this large trial, that combining this targeted therapy with hormone treatment may help to delay or even stop cancer coming back. This will require further research to confirm, however these results are a vital step forward tackling one of the major challenges that we encounter with breast cancer.”
Professor Judith Bliss, Director of the Clinical Trials and Statistics Unit at The Institute of Cancer Research, London, who led the management of the study, said:
“Hormone therapy is very effective in hormone receptor-positive breast cancer, but tumours can evolve resistance to treatment – and women are often left with anxiety about the possibility that their cancer will come back.
“Our new trial analysed tumour samples taken at various points during women’s treatment with hormone therapy and the targeted drug palbociclib – allowing us to get a detailed picture of women’s response to the drug on a biological level.
“Our study showed that adding palbociclib to hormone therapy slows cancer cell growth, which for other treatments can be an important molecular clue that can help predict the length of time before breast cancer returns. Other studies will show whether treatment with palbociclib can deliver on its promise by delaying cancer’s relapse.”
Important reduction in cancer cell growth
Professor Mitch Dowsett, Professor of Biochemical Endocrinology at The Institute of Cancer Research, London, and Head of The Royal Marsden Ralph Lauren Centre for Breast Cancer Research, said:
“This new clinical trial has found that adding the targeted treatment, palbociclib, to hormone therapy at diagnosis leads to an important reduction in cancer cell growth, and in many women stops it entirely.
“While adding palbociclib to treatment with an aromatase inhibitor did not translate to a decrease in the size of women’s tumours, we identified important molecular clues to help assess how palbociclib affects cancer cell growth.
“In future, the tumour samples collected during this trial could also allow us to analyse the genetic make-up of women’s tumours, which could help pick out those women most likely to benefit from the drug.”
Kathryn England, 62, a Grandmother from Sutton, was diagnosed with breast cancer in March 2015 and immediately went on to the PALLET trial at The Royal Marsden. She said:
“After three months, the drugs had made one tiny tumour disappear and had shrunk the larger one. I then had a lumpectomy and radiotherapy, and have been clear of cancer for three years now. Without the trial I might have had to have chemotherapy.
“Instead, I didn’t lose my hair, I was able to carry on working and my lifestyle didn’t change that much. But the most important thing is that it worked for me.”