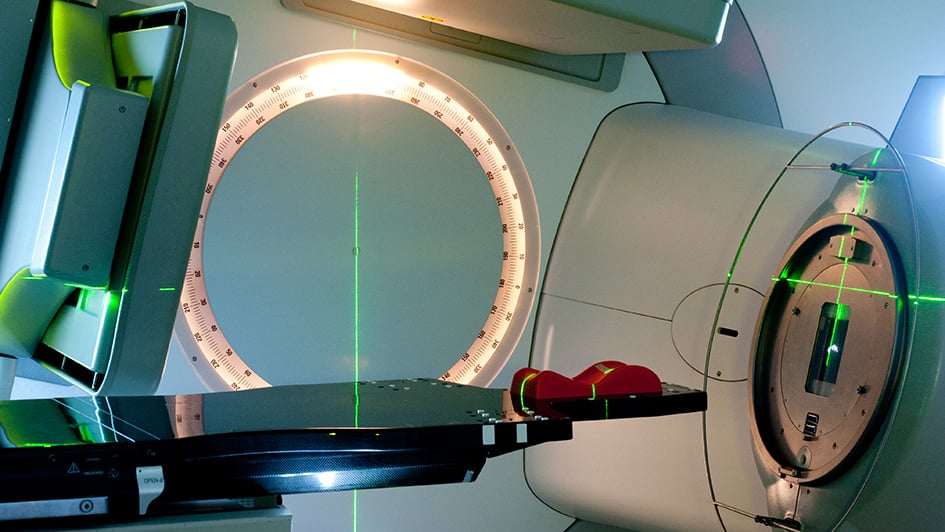
 Image: A radiotherapy machine.
Image: A radiotherapy machine.
Researchers are a step closer to revolutionising how doctors use radiotherapy to treat patients with muscle-invasive bladder cancer.
A team of scientists, led by The Institute of Cancer Research, London, have shown that personalised radiotherapy – in which the radiotherapy is tailored specifically to an area of the patient’s body – offers a potentially kinder way of treating people with bladder cancer.
The work was funded by Cancer Research UK, Cancer Australia and the Cancer Society of New Zealand and is described in a paper published in the journal European Urology.
Professor Robert Huddart, Professor of Urological Cancer and Honorary Consultant Clinical Oncologist at the Royal Marsden and Group Leader at The Institute for Cancer Research, London, said:
“Delivering radiotherapy to the bladder is a challenging process. We are pleased this work into a potential new way of treating bladder cancers has allowed us to deliver effective treatment safely and allowed us to use a high dose which promises to cure more patients, with relatively few long-term side effects.
“We look forward to studying this method further to explore its effectiveness versus current treatment options.”
Healthcare workers face a number of challenges treating muscle-invasive bladder cancer including the aggressive nature of the disease as well as the bladder changing shape and position which creates complications when delivering targeted radiotherapy.
Modern radiotherapy is a cornerstone of cancer medicine, with around three in 10 patients receiving it as part of their primary treatment. It works by targeting tumours with X-ray radiation, killing cancer cells by irreversibly damaging their DNA.
Today, over 130,000 patients are treated with radiotherapy on the NHS every year, but the current use of the treatment typically involves a ‘one size fits all’ approach, in which the dosage is the same in each session, which can limit the success of the therapy when targeting areas of the body that change and move.
That could all change with the introduction of personalised treatments, such as ‘adaptive’ radiotherapy. That method involves changing the volume of radiotherapy to be delivered depending on the area of the body being targeted, rather than giving the same volume in each session.
The Phase 2 RAIDER study was designed to find out whether it is possible to deliver adaptive radiotherapy to treat muscle-invasive bladder cancer, which involved creating three treatment plans (small, medium and large) and then choosing the one that best fits the size and position of the patient’s bladder at each treatment appointment. The work took place in the UK, Australia and New Zealand.
In total, 345 patients were split into one of three groups, each receiving a different course of treatment. The first group received standard radiotherapy treatment, i.e. the same treatment plan in each session, while the other two groups received one of a number of treatment plans, determined on a case-by-case basis in each session. One of these groups also had a higher-than-normal radiation dose.
Study participants were asked about any side effects they experienced post-treatment, as well as questions about their general quality of life. The researchers found that across all groups of patients, there were fewer serious long-term side effects six to 18 months after treatment than those reported in previous studies. There was no evidence that those who received higher dose treatment had any worse side effects compared with those who received standard radiotherapy treatment. This could potentially lead to a kinder and more effective form of radiotherapy for this type of cancer if approved.
Professor Emma Hall, Co-Director of the Cancer Research UK-funded Clinical Trials and Statistics Unit and Group Leader at The Institute for Cancer Research, London, said:
“As medical technologies continue to improve, it means that we can investigate delivering more complicated and personalised forms of radiotherapy to treat certain cancers.
We are grateful to those who took part in the RAIDER study, allowing us to determine if adaptive radiotherapy can be given to patients with bladder cancer without substantially worsening their quality of life post-treatment.”
The RAIDER study was also supported by the National Institute of Health and Care Research Biomedical Research Centre at The Royal Marsden NHS Foundation Trust.
The trial was not designed to examine whether this way of giving radiotherapy was more effective at treating the patients’ cancer, but further studies are planned to confirm this.
Dr Hattie Brooks, Research Information Manager at Cancer Research UK, said:
“It’s exciting to see the potential of adaptive radiotherapy to treat bladder cancer. Although still in the clinical trial stage, this new targeted radiotherapy approach could reduce side effects for people being treated for the disease. We look forward to following the next part of this work to further assess the treatment effectiveness and benefits of adaptive radiotherapy.
With projects like the RAIDER study, we’re accelerating the development of more personalised and kinder treatments so that more people can live longer, better lives free from the fear of cancer.”
The paper, titled “Dose-escalated adaptive radiotherapy for bladder cancer: results of the phase II RAIDER randomised controlled trial” was published today (7 Oct) in European Urology.
.tmb-propic-md.jpg?Culture=en&sfvrsn=492e618f_9)
 .
.
 .
.