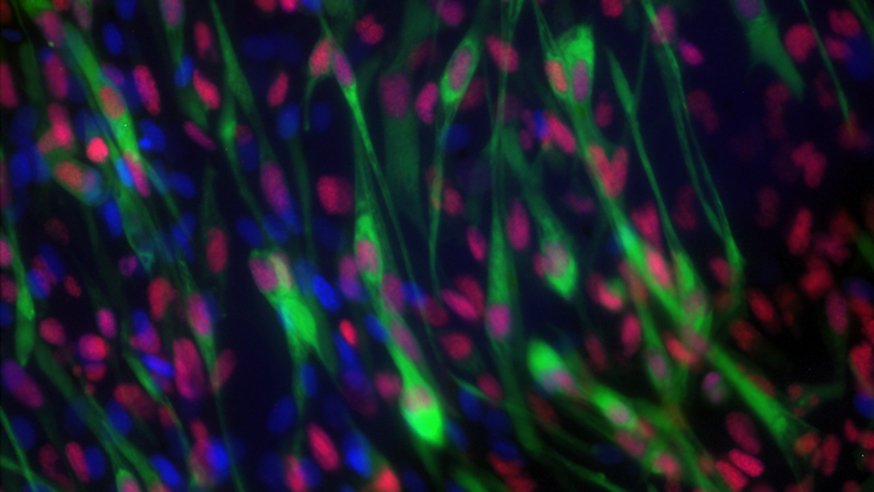
Image: Rhabdomyosarcoma cells. Credit: Dr Ewa Aladowicz, ICR
A new study could lead to improved decision making in assigning treatments for children with the aggressive cancer rhabdomyosarcoma after revealing key genetic changes underlying development of the disease.
In the largest and most comprehensive study of rhabdomyosarcoma to date, scientists found that specific genetic changes in tumours are linked to aggressiveness, early age of onset and location in the body.
All these factors affect the chances that children will survive their disease – and understanding how they are driven by a cancer’s genetics could lead to new ways of tailoring treatment for each patient.
Rhabdomyosarcoma is a rare type of cancer that resembles muscle tissue and mostly affects children. Less than 30 per cent of children with rhabdomyosarcoma who have relapsed or whose cancer has spread will survive.
'Could be spared the most severe side effects'
The new international study, led by researchers at The Institute of Cancer Research, London, could help pick out children with particularly aggressive cancers in need of intense treatment and close monitoring.
It could also identify other children who could benefit from less aggressive therapy and could be spared some of the most severe side effects of treatment.
The researchers are already planning to incorporate the new insights into the design of upcoming clinical trials aiming to improve the management of the disease.
The international group of researchers analysed the DNA from 641 patients with rhabdomyosarcoma. The study was published in the Journal of Clinical Oncology and was funded by Cancer Research UK and several charities who fundraise specifically for research into rhabdomyosarcoma – the Chris Lucas Trust, Talan’s Trust and Alice’s Arc.
Two main sub-types of rhabdomyosarcoma exist – fusion gene-positive and fusion gene-negative, depending on the presence of a ‘fusion gene’. A fusion gene is a hybrid gene formed from two previously separate genes – in this case, a PAX gene and a gene called FOXO1.
Looking at MYOD1 and TP53 mutations
When looking at children with fusion-negative rhabdomyosarcoma, researchers found that children whose tumours had faults in the genes MYOD1 and TP53 had significantly poorer response to treatment and worse survival outcomes. TP53 was altered in 69 out of 515 children and was linked to worse survival outcomes.
Approximately half the children whose cancers had TP53 mutations succumbed to their disease compared with one in four children with cancers that were not TP53 mutant – indicating that those without the mutation had a better chance of survival.
The researchers found mutations in MYOD1 in 17 out of 515 children and linked these to both worse outcomes and rapid progression of the disease. The findings suggest that children with these mutations could benefit from more aggressive treatment.
A small number of children with fusion-positive rhabdomyosarcoma – five out of 126 – also had changes in TP53. None of these children survived their cancer and, as a consequence, researchers have identified TP53 as a ‘high risk’ indicator in this sub-group too.
CDK4, MYCN and RAS mutations
Researchers believe having too many copies of the genes CDK4 or MYCN may also be linked to a poorer outcome in fusion-positive rhabdomyosarcoma, with 16 and 13 cases, respectively, showing these genetic changes. However, as the number of cases in the study was small this needs to be explored further in future research.
The new study challenges previous findings that the presence of a fault in the RAS gene is linked to poor outcomes. Researchers did however find that some RAS mutations seemed to be correlated with particular ages of onset – with HRAS mutations arising in babies, KRAS mutations in toddlers and NRAS mutations in adolescence.
Babies have previously been shown to have lower survival than older children, which may be because clinicians avoid using more aggressive treatments like radiation in the youngest patients.
Taking into account findings from this study, researchers believe that using targeted drugs such as tipifarnib, which blocks HRAS, may be particularly beneficial for these young, vulnerable and high-risk patients.
Helping guide treatment
Study leader Professor Janet Shipley, Professor of Molecular Pathology at The Institute of Cancer Research, London, said:
“Our findings shed light on the genetic changes that underlie rhabdomyosarcoma, a rare and aggressive childhood cancer. By looking at the genetic features of different tumours, we can divide children into different risk groups to help guide their treatment.
“Decades of clinical trials have led to the current complicated system for assigning risk to children with rhabdomyosarcoma – but we know that the current system is not accurate enough to properly assign treatment for individual children. Our findings should refine the current system and treatments clinicians provide to more effectively match each child’s genetic profile and risk. Ultimately, further research may highlight new drugs to tailor treatment for patients with high-risk rhabdomyosarcomas that have specific genetic defects.”
An international collaborative effort
Professor Paul Workman, Chief Executive of The Institute of Cancer Research, London, said:
“This international collaborative effort has linked specific genetic changes in cancers to the ways that children respond to treatment. It should help clinicians to treat children according to the particular features of their cancer and the risk they face of their cancer progressing. The findings have the potential to have a real impact not only on survival but also on quality of life, by picking out those children who need the most aggressive treatment, but also sparing others with lower-risk disease from the side effects of intensive interventions.”
'To defeat this devastating childhood cancer'
Alice’s Arc was inspired by Sara’s and David’s daughter Alice who, at the age of three, was diagnosed with rhabdomyosarcoma. Alice's Arc was established just after her diagnosis. Alice died four and half years later, aged just seven. Sara Wakeling, Co-founder of Alice's Arc, said:
"We believe the future of treating rhabdomyosarcoma effectively and kindly is reliant on understanding the features of each individual's tumour and tailoring treatment accordingly. We are delighted to have played a role in helping to build understanding of these genetic features of rhabdomyosarcoma tumours and how they play a part in predicting outcomes and influencing treatment pathways. We look forward to continuing to work with the team at the ICR to uncover more clinically translatable research discoveries to defeat this devastating childhood cancer."
We have made huge progress in cancer treatment over the years, but there continue to be cancers that have poor survival rates, such as advanced bowel cancer, the second most common cause of cancer death in the UK. Your support today will help us develop smarter treatments for bowel cancer patients and give these patients hope for the future.
