Sarcoma Molecular Pathology Team
Professor Janet Shipley’s team is investigating ways to improve the treatment of patients with soft tissue sarcomas associated with poor clinical outcome.
Our current research is primarily focused on rhabdomyosarcomas and includes understanding aspects of epigenetic regulation of differentiation and the DNA damage response that may be targeted and incorporated into the treatment of these and other sarcomas.
Professor Janet Shipley
Group Leader:
Sarcoma Molecular Pathology, Computational Pathology and Integrative Genomics
Professor Janet Shipley is investigating ways to improve the treatment of patients with sarcomas that have a poor outcome.
Rhabdomyosarcoma (RMS)
RMS account for around 6% of all childhood cancers and are broadly divided into two main histological subgroups: alveolar and embryonal RMS. Around 70–80% of alveolar cases are associated with PAX3/FOXO1 or PAX7/FOXO1 gene fusions.
Our work has shown that fusion gene negative alveolar RMS are clinically and biologically more similar to embryonal cases than alveolar and patients with PAX3/FOXO1 positive tumours are associated with poorer outcome.
This has important implications for risk stratification that are being incorporated into the next clinical trial by the European paediatric Soft tissue sarcoma Study Group (EpSSG). In addition, we have identified a gene signature associated with poor prognosis in fusion gene negative RMS that will be prospectively validated.
To find new approaches to treat these high-risk sarcoma patients we are identifying and validating:
- Molecular therapeutic targets and agents that are prioritised from a novel computational analyses of molecular and experimental data (in collaboration with Professor Bissan Al-Lazikani). These are then being tested in our preclinical models.
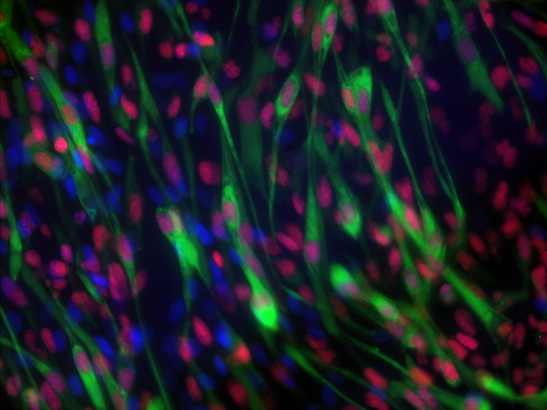
- Epigenetic modifying enzymes that have effects on the differentiation status or DNA damage response of RMS cells. These include the histone demethylase KDM4 family that is linked to a drug discovery project (collaboration with Professor Julian Blagg) and the histone methyl transferase EZH2 which is part of the polycomb repressive complex 2 (in collaboration with Dr Zoe Walters). This research aims to discover novel strategies for differentiation therapy and ways to make sarcoma cells more sensitive to current treatments which damage DNA.
Other sarcomas
Our research investigations are extended to desmoplastic small round cell tumours, liposarcomas, Ewing sarcomas and through collaboration with Professor Chris Lord, synovial sarcomas.
We have close links with clinicians at the Royal Marsden NHS Foundation Trust (in the Children and Young People's Unit and the Sarcoma Unit), the National Cancer Research Institute (NCRI) Clinical Studies Young Onset Sarcoma Subgroup (YOSS) and the European paediatric Soft tissue sarcoma Study Group (EpSSG).
These partnerships facilitate our research and take forward research advances to potentially benefit patients.
Research Support
Support for our sarcoma research has come from:
- Sarcoma UK
- Children with Cancer UK
- The Chris Lucas Trust
- RobsARTTT
- Great Ormond Street Hospital Charity
- The Tom Bowdidge Foundation
- Cancer Research UK
- Wellcome Trust
- Elin Rose Appeal
- Kidscan
- Children’s Cancer & Leukaemia Group
- The Kelly Turner Foundation
- Alice's Arc
- Leah Rothwell
- Charlie's Wish
The aim of the Sarcoma Molecular Pathology Group is to identify molecular biomarkers of high-risk sarcomas and therapeutic strategies that will improve the treatment of patients with these sarcomas.
Sarcomas are a heterogeneous group of mesenchymal tumours that frequently exhibit features of differentiating tissues such as striated skeletal muscle (rhabdomyosarcomas) and fat (liposarcoma). They may also have an undifferentiated appearance. Sarcomas account for approximately 15% of cancers in children and adolescents compared with 1% of cancer in adults and are associated with considerable morbidity and mortality.
Our current research is primarily focused on rhabdomyosarcomas and includes understanding aspects of epigenetic regulation of differentiation and the DNA damage response that may be targeted and incorporated into the treatment of these and other sarcomas.
Previously, we have identified genes involved in testicular germ cell tumour development, including those that predict occult spread and relapse. Other research has led to the identification of rearranged genes, notably those involved in synovial sarcomas, chondrosarcomas, kidney carcinomas and a myeloproliferative disorder.
We have also derived genetic-based approaches to resolve diagnostic dilemmas for the differential diagnosis of small round cell tumours, synovial sarcoma and tumours of germ cell origin. More recently, we demonstrated that the PAX3-FOXO1 fusion gene, rather than alveolar histology, is a key prognostic marker with utility to stratify treatment for rhabdomyosarcoma patients.
Recent discoveries from this group