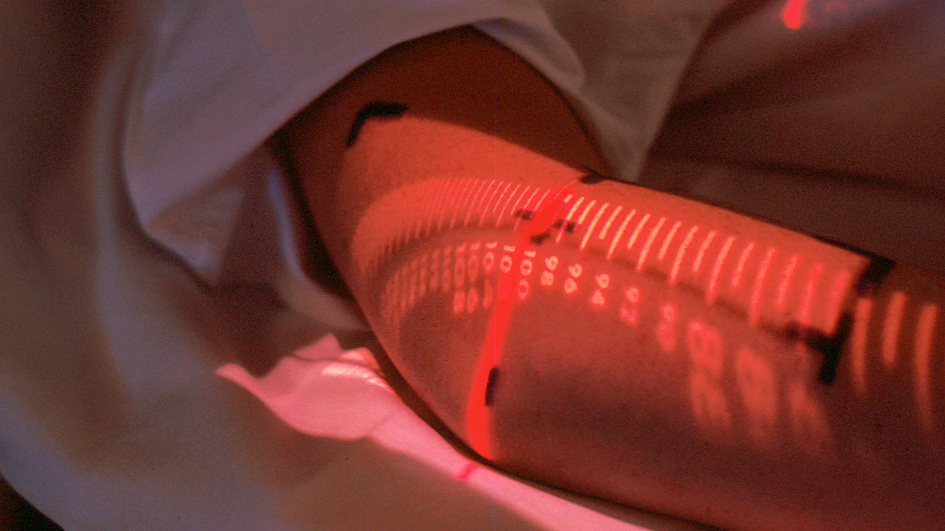
Image: Pre-measurement for Radiation Therapy: a lighted scale is projected onto the body to exactly line up the treatment with the tumour site. Credit: National Cancer Institute
Data from a clinical trial which assessed the benefits of adding chemotherapy alongside radiotherapy for patients with muscle invasive bladder cancer has shown that this treatment can be given without substantially impacting subsequent health related quality of life.
Patients who received chemotherapy alongside radiotherapy were surveyed about their quality of life with regard to their health at the end of their treatment, and at six, 12, 24, 36,48 and 60 months after treatment.
In this phase III trial, jointly led by researchers at The Institute of Cancer Research, London and the University of Birmingham, patients with muscle invasive bladder cancer were randomised to receive radiotherapy with or without chemotherapy, alongside different types of radiotherapy to the bladder.
Improving quality of life over the long term
Results previously showed that adding chemotherapy to radiotherapy as part of the treatment regimen for this cancer type halves the risk of the cancer returning. Patients given a low dose of chemotherapy alongside radiotherapy were nearly 50 per cent less likely to relapse with the most lethal form of the disease compared to patients given radiotherapy alone.
This study, published in the journal European Urology, examined data from patient questionnaires which were answered in the clinic before treatment began, at the end of treatment, at a six-month follow up and then every year for five years.
Patients were asked to answer 39 different questions relating to their quality of life and wellbeing. Four-hundred and fifty two participants from 45 UK NHS Trusts completed at least one questionnaire during the study.
The research showed that while patients understandably report a negative impact on their quality of life at the end of treatment, over the long term, patients on average had maintained or improved quality of life on follow up.
We have a proven track-record of awe-inspiring research, which is transforming the lives of cancer patients around the world. This work is made possible by an extraordinary community of generous donors, which includes individuals, trusts and foundations and charity partners.
While the overall picture is positive, with the majority of patients reporting quality of life similar to or better than their quality of life prior to treatment, some patients do experience a substantial decline in quality of life.
Importantly, patients who receive chemotherapy in conjunction with radiotherapy have either the same or better health-related quality of life as patients who just received radiotherapy on its own.
Sparing many patients from invasive surgery
Professor Robert Huddart, Professor of Urological Cancer at the ICR, and Consultant in Urological Oncology at The Royal Marsden NHS Foundation Trust, said:
“We have shown that the addition of chemotherapy to radiotherapy in the treatment of muscle invasive bladder cancer significantly improves clinical outcomes for patients, and spares many patients from invasive surgery.
“Although patients report a drop in quality of life as they deal with side effects immediately following treatment, we are pleased to see this levels out over the course of the following years and the addition of chemotherapy doesn’t seem to impair quality of life.
“Understanding what drives the deterioration in quality of life seen in some patients should be a priority for future research in bladder cancer.”
Professor Emma Hall, Deputy Director at the ICR Clinical Trials and Statistics Unit and methodology lead for the study said:
“Understanding the impact of new treatments on patients is important in understanding the risk:benefit ratio and supporting informed treatment choices.
“A recently awarded Cancer Research UK Clinical Trials Unit Fellowship will build on these findings to explore efficient ways to assess treatment related side effects in other bladder and prostate radiotherapy clinical trials”.