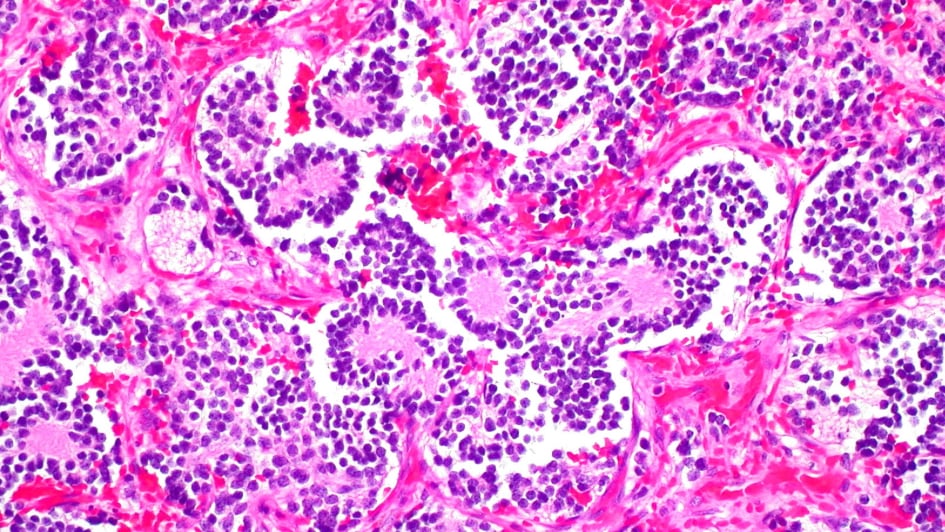
Image: Neuroblastoma of the adrenal gland. Credit: Ed Uthman. CC BY-NC 2.0
Neuroblastoma is the most common childhood cancer, and each year, around 100 families will receive the terrible news that their child has been diagnosed.
It originates from a type of nerve tissue that doesn’t stop growing after early development in the womb. Tumours usually form in the abdomen, near the kidneys, but they can also form closer to the spine, neck or chest.
Treatment for neuroblastoma depends on the aggressiveness of the tumour. Although many children will be cured after chemotherapy and surgery, around half of children will have what is considered high-risk disease.
High-risk neuroblastoma is often driven by specific genetic mutations and is much harder to treat – children often have to undergo very intensive treatments, which do not always work - and sadly around half of children diagnosed with high-risk neuroblastoma do not survive past five years. Those who do survive may be left with lifelong side effects from the lifesaving but harsh treatment they received. There is a huge need for more effective, targeted and less toxic treatments.
Scientists have already started to achieve this. One of the most significant recent developments in the treatment of neuroblastoma is the introduction of an immunotherapy drug called dinutuximab, which was made available on the NHS for children with high-risk neuroblastoma in 2018 following positive clinical trial results.
Dinutuximab is a monoclonal antibody – a type of biological drug that uses synthetic versions of antibody proteins normally found in the immune system.
This cutting-edge immunotherapy seeks out neuroblastoma cancer cells by sensing a protein on their surface called GD2, destroys them, and sparks the immune system into action to further wipe out cancer cells.
Clinical trials estimate that adding dinutuximab to treatment can reduce the risk of cancer recurring after 70 months (5.8 years) by 32 per cent and improve children's chances of being alive after 70 months by 37 per cent.
A global research effort
At The Institute of Cancer Research, London, we're part of a global team of scientists who are working together to find more effective, targeted and less toxic treatments for neuroblastoma.
In the UK, most children diagnosed with neuroblastoma will receive their treatment at specialist cancer centres on clinical trials, which are constantly adapting to advances. Thanks to this participation and to ongoing research efforts by scientists, the last five years have seen real scientific progress in neuroblastoma treatment.
Last year was a big year for clinical trials in neuroblastoma, with several new treatments showing promise against the disease. These advances in treatment are granting children extra weeks or months with their loved ones, and in some cases, helping cure more children of their cancer.
Lorlatinib – exciting results in clinical trials
In early 2023, a major clinical trialshowed that a new drug called lorlatinib – originally developed to treat adult lung cancers – showed great promise for treating the childhood cancer neuroblastoma in cases where it is driven by a specific mutation in a protein called ALK.
Neuroblastomas are often driven by specific genetic alterations, including in the ALK gene, that fuel their growth. At diagnosis, up to 15 per cent of patients with neuroblastoma have the rearranged ALK gene. These mutations often occur in high-risk neuroblastoma and children whose cancers have relapsed often have more of them within their tumours. In the clinic, doctors can test for these mutations and identify which patients might benefit from specific treatments.
The international trial was led by a group of researchers in the US, including the Children’s Hospital of Philadelphia (CHOP), as part of the New Approaches to Neuroblastoma Therapy (NANT) Consortium – a global group of universities and children's hospitals that works to develop new treatments and tests for neuroblastoma.
Professor Louis Chesler, Professor of Paediatric Cancer Biology at the ICR and Dr Lynley Marshall, who is clinical lead of the Centre for Paediatric Oncology and Experimental Medicine (POEM) at the ICR and the Royal Marsden, were the UK-leading members of this global research group.
Findings of the NANT trial
The phase I trial looked at giving lorlatinib either alone or in combination with chemotherapy to both children and adults with ALK-positive neuroblastoma that had relapsed on standard treatments.
Around 30 per cent of children who received lorlatinib saw their tumours respond to the drug. It was particularly effective for children when used in combination with chemotherapy. The data showed that 63 per cent of children who received the combination treatment had a response, meaning their tumours shrank.
Among the participants aged over 18, lorlatinib alone produced a response rate of 67 per cent.
Following these results, from next year, all children newly diagnosed with neuroblastoma with ALK mutations will receive lorlatinib as a first line treatment as part of a phase III clinical trial, to be conducted in both North America and Europe. It's hoped more children will be cured of their disease.
Overcoming resistance to lorlatinib
Like all cancer drugs, lorlatinib can stop working and the disease can relapse after treatment. Our scientists are carrying out an extensive programme of research to understand why neuroblastomas become resistant to treatments such as lorlatinib and identify new strategies to keep them working for longer.
Early findings from our scientists suggest that combining lorlatinib with another type of drug called an MDM2 inhibitor could prove a promising treatment strategy. Studies in mice showed that combining the two drugs kept them working for much longer. ICR scientists will continue to uncover new vulnerabilities in neuroblastomas, hopefully paving the way to more effective treatment combinations and more cancer cures.
Dr Lizzie Tucker, a Postdoctoral Training Fellow at the ICR who is studying in the lab how neuroblastoma develops resistance to treatment, said:
"The past year has been incredibly exciting for neuroblastoma research. Lorlatinib has been a real standout drug and it's wonderful that lorlatinib was so effective for patients with this specific mutation. It's not to say it is a wonder drug – it does not work for every patient, and we still need to find ways in the lab to make it more effective, but it's extremely promising. At the ICR, we are working to develop new treatments that exploit other mutations within neuroblastoma, particularly the MYCN gene, which we know drives aggressive neuroblastoma in many children. This would open up a personalised treatment option for more children."
CAR T-cell therapy
CAR T-cell therapy is a revolutionary type of cancer treatment that is already being used to treat patients with blood cancer. These therapies are currently being explored in early trials of patients with high-risk neuroblastoma.
In April last year, scientists showed that CAR-T cell therapy could be effective against neuroblastoma. It was the first time scientists had shown CAR-T therapy could be effective for solid tumours. The findings were published in the New England Journal of Medicine.
This cutting-edge type of immunotherapy involves taking a patient's own immune cells, reprogramming them in the lab to recognise and attack cancer cells, and then reinfusing them into a patient's bloodstream where they seek out and destroy cancer cells.
In the trial, 63 per cent of neuroblastoma patients who had exhausted most other treatments and seen their tumours relapse responded to the treatment, meaning their tumours shrank. In addition, in many cases, the CAR T-cells remained in the blood for several months, where they may have continued to recognise and wipe out cancer cells.
Scientists specifically designed the treatment to selectively target cancer cells by seeking out a protein called GD2, which is found at higher levels on the surface of neuroblastoma cells than it is on healthy cells. Dinutuximab, the immunotherapy drug that has been used to treat NHS patients with neuroblastoma since 2018, targets the same protein.
Larger clinical trials are continuing to explore the safety, benefits and feasibility of using CAR-T therapy in neuroblastoma.
Targeting tumour blood supply with bevacizumab
In January this year, results from an international clinical trial showed that combining drugs that prevent tumours from growing blood vessels, also called anti-angiogenic drugs, with chemotherapy helped more children respond to treatment.
Anti-angiogenic drugs limit blood supply to tumours and therefore restrict their growth.
The study, led by the Cancer Research UK Clinical Trials Unit (CRCTU) at the University of Birmingham, involved 160 children and young people across Europe. Half of the children received conventional treatment, and half received conventional treatment alongside bevacizumab. Children who received bevacizumab were more likely to see their tumours shrink – 26 per cent of children who received bevacizumab responded to treatment compared with 18 per cent of those who received the standard of care.
The findings were published in the Journal of Clinical Oncology, and the combination treatment has already been incorporated into the UK standard of care guidelines for neuroblastoma treatment, meaning all eligible children will receive bevacizumab as part of a clinical trial.
Other promising research
There are many promising avenues of research into neuroblastoma. It's not just about discovering new treatments but also fine-tuning and improving how we use the treatments we already have.
Some of these avenues include testing whether combining different chemotherapy drugs could increase the effectiveness of treatment and whether giving existing drugs at different times could make them more effective.
With each new discovery, scientists hope to make incremental improvements in survival rates for neuroblastoma.
There are also major efforts to find ways to make treatments gentler, so that more children are spared from the lifelong side effects of intensive treatments.
With global efforts to improve the lives of children diagnosed with neuroblastoma, we're confident that the coming decades will bring a new pipeline of discoveries and new treatments.
Our scientists have led major studies and clinical trials of new drugs for neuroblastoma and have developed gene tests that the NHS now uses to better match patients to targeted drugs that exploit the individual biology of their tumours, and we're building on these tests and treatments.
We co-lead the Stratified Medicine Paediatrics (SMPaeds2) initiative - a programme of molecularly profiling children's tumours at diagnosis and relapse to provide information that can help doctors match patients to the best treatment for their individual cancer.
SMPaeds2 is funded by Cancer Research UK and is building on the successes of Stratified Medicine Paediatrics 1 (SMPaeds1) which set up the UK’s first National Molecular Tumour profiling platform for children whose cancers had relapsed.
The SMPaeds2 initiative involves analysing children's tumours in even more detail to uncover new insights into the biology of the disease and pave the way to better precision medicines. It's also helping to develop less invasive testing, by advancing the use of 'liquid biopsies' - tests which detect tumour DNA in the blood and other body fluids, therefore avoiding the need for invasive biopsies. It's hoped these tests could be used to match children to personalised treatments, monitor how well treatments are working in real time, and allow faster detection of relapse.
Professor Louis Chesler leads the Paediatric Solid Tumour Biology and Therapeutics Team at the ICR and co-leads the SMPaeds initiatives. He said:
"Here at the at the ICR, we're proud to be part of worldwide efforts to push forward scientific advances and transform the lives of children diagnosed with neuroblastoma. Exciting developments over the last five years show us just how much research can transform the outlook for patients with neuroblastoma, but there are still many children who will run out of treatment options and sadly die from the disease. We're determined to change this.
"We're proud to lead an intensive research programme here at the ICR to develop better, less toxic, personalised treatments for neuroblastoma which carry fewer side effects. We're grateful to all our supporters. Donations towards our world-leading research will paint a brighter future for children with neuroblastoma and their families."
The ICR is part of a global team of scientists who are working to discover more effective, kinder treatments and to give more children the chance of a cure. We need your help.