An innovative light-activated therapy developed at The Institute of Cancer Research, London, could help detect and treat an aggressive brain cancer type, a new study shows.
The ‘photoimmunotherapy’ combines a special fluorescent dye with a cancer-targeting compound, which together boosts the body’s immune response.
In studies in mice, the combination was shown to improve the visibility of cancer cells during surgery and, when activated by near-infrared light, to trigger an anti-tumour effect.
The treatment, studied by an international team of researchers from the ICR and the Medical University of Silesia, Poland, could ultimately help surgeons to remove brain cancers like glioblastoma more effectively, and boost the body’s response to cancer cells that remain after surgery.
The study was largely funded by the Cancer Research UK Convergence Science Centre at the ICR and Imperial College London – a unique partnership that is bringing together scientists from the engineering, physical and life sciences to develop innovative ways to address challenges in cancer. It was also supported by the Swedish company AffibodyAB.
Lighting-up brain cancer
Glioblastoma multiforme, also known as GBM, is one of the most common and aggressive types of brain cancer. New ways to improve surgery could help patients live for longer.
Surgeons often use a technique called Fluorescence Guided Surgery to treat diseases like glioblastoma and other brain cancers, which uses dyes to help identify the tumour mass to be removed during surgery.
But due to these tumours growing in sensitive areas of the brain like the motor cortex, which is involved in the planning and control of voluntary movements, glioblastoma surgery can leave behind residual tumour cells that can be very hard to treat – and which mean the disease can come back more aggressively later.
The new research, published in the journal BMC Medicine, builds on Fluorescence Guided Surgery using a novel technique called photoimmunotherapy (PIT).
This treatment uses synthetic molecules called ‘affibodies’– small proteins engineered in the lab to bind with a specific target with high precision.
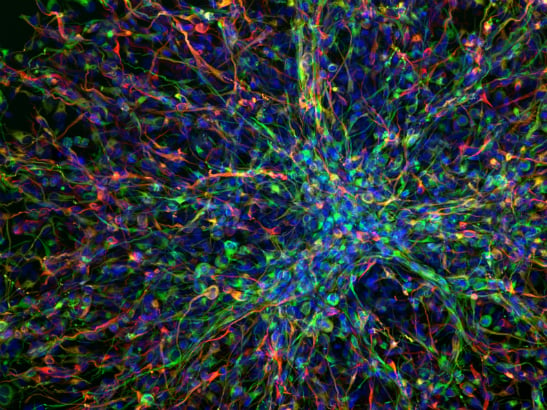
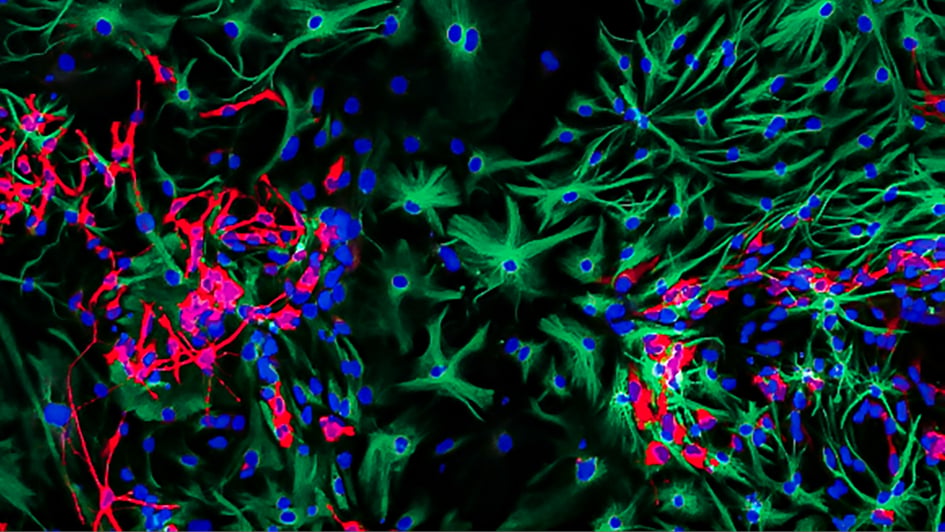
In this study, the researchers combined an ‘affibody’ created to recognise a protein called EGFR – which is mutated in many cases of glioblastoma – with a fluorescent molecule called IR700, which is used in surgery.
Shining light on these compounds causes the fluorescent dye to glow, highlighting microscopic regions of tumours left in the brain, while switching to near-infrared light triggers anti-tumour activity that kills tumour cells.
Offering new hope for brain cancer
The researchers tested this combined molecule, or ‘conjugate’ – known scientifically as ZEGFR:03115-IR700 – in mice with glioblastoma. They could see the cancer-targeting compound fluorescing in the brain tumours during surgery, just one hour after administration.
Shining near-infrared light on the tumour cells then activated the anti-tumour effect of the compound, killing cancer cells: scans of mice treated with the compound showed distinct signs of tumour cell death compared with untreated mice.
Photoimmunotherapy also triggered immune responses in the body that could prime the immune system to target cancer cells, so the treatment could help prevent glioblastoma cells from coming back after surgery.
As well as being a possible future treatment for glioblastoma, the approach used for ZEGFR:03115-IR700 could also be adapted against other targets in other forms of cancer, using new affibody molecules.
Researchers at the ICR are now also studying the treatment in the childhood cancer neuroblastoma.
Study leader Dr Gabriela Kramer-Marek, Team Leader in Preclinical Molecular Imaging at the ICR, said:
“Brain cancers like glioblastoma can be hard to treat and sadly, there are too few treatment options for patients. Surgery is challenging due to the location of the tumours, and so new ways to see tumour cells to be removed during surgery, and to treat residual cancer cells that remain afterwards, could be of great benefit.
“Our study shows that a novel photoimmunotherapy treatment using a combination of a fluorescent marker, ‘affibody’ protein and near-infrared light can both identify and treat leftover glioblastoma cells in mice. In the future, we hope this approach can be used to treat human glioblastoma and potentially other cancers too.”
As well as being a world leading cancer research organisation, we are a charity. With the help of people like you, our research is helping patients live longer and live well with cancer. Support our research today to unlock new combination treatments, so more people will survive cancer.
Professor Axel Behrens, Scientific Director of the Cancer Research UK Convergence Science Centre at the ICR and Imperial College London, and Leader of the Cancer Stem Cell Team at the ICR, said:
“Multidisciplinary working is critical to finding innovative solutions to address the challenges we face in cancer research, diagnosis and treatment – and this study is a great example of how researchers at our centre are working across traditional discipline boundaries. This research demonstrates a novel approach to identifying and treating glioblastoma cells in the brain using light to turn an immunosuppressive environment into an immune-vulnerable one, and which has exciting potential as a therapy against this aggressive type of brain tumour."