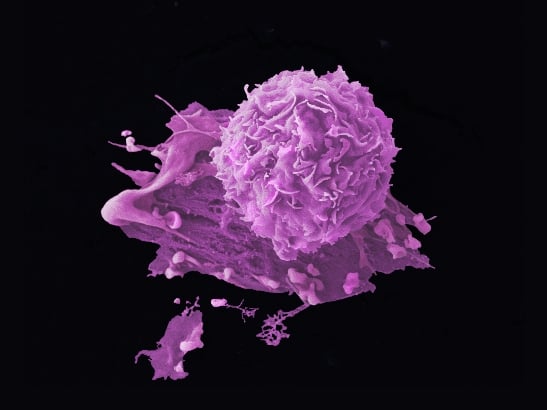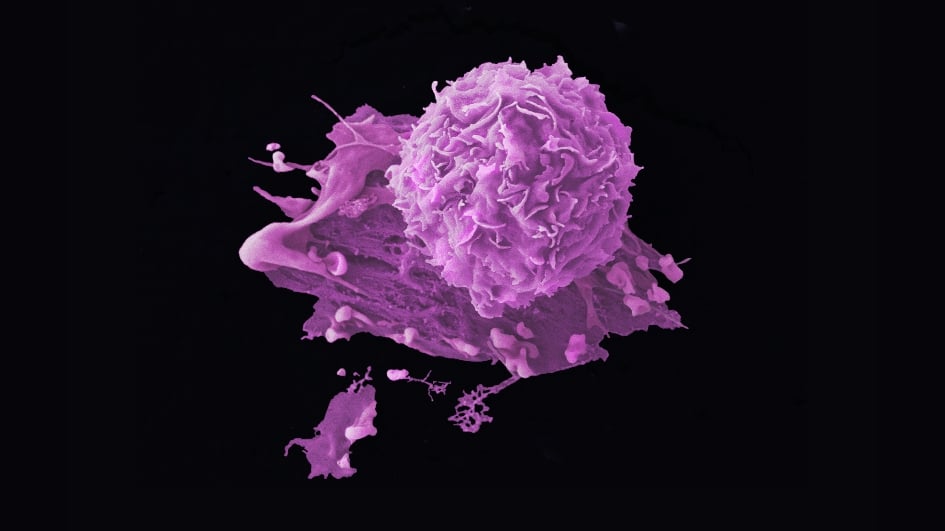
Researchers have performed a deep dive into the different immune markers within tumour tissue and blood samples of early breast cancer patients whose cancer failed to respond to chemotherapy given to them prior to surgery.
The research gives insight into the function of immune cells in patients with chemotherapy-resistant breast cancers. While chemotherapy may not kill cancer cells in these high-risk patients, immunotherapy, a type of treatment that helps the immune system to attack cancer cells, may provide a benefit.
Effects of chemotherapy on immune cells
To investigate the immune environment that surrounds these chemotherapy-resistant tumours, researchers from King's College London and The Institute of Cancer Research, London, employed multiple and novel complementary technologies looking at proteins and genes on both pre-treatment and post-treatment breast cancer tissue. They also measured how 1,330 cancer and immune-related genes within cancer tissues were affected by chemotherapy.
They found that chemotherapy-resistant cancer cells had very few immune cells around them, but chemotherapy did induce changes in several immune cell types. Specifically, they found increases in the number of “innate” (first responder) cells such as neutrophils and natural killer (NK) cells. NK cells help the body to fight infection and cancer. But analysis found the increased NK cells in patients with chemotherapy-resistant disease lacked cytotoxic activity – the ‘killing instinct’.
Developing immunotherapies for high-risk breast cancer patients
The researchers, largely funded by Breast Cancer Now, also found immune-related genes associated with NK cells were those associated with cell inhibition or exhaustion, which meant NK cells were unable to fight cancer cells. This new insight into the behaviour of NK cells could be used to develop specific immunotherapies for these high-risk patients. This would need to be investigated in future clinical trials.
These findings, published in Clinical Cancer Research, a journal of the American Association for Cancer Research, also show that blood monitoring during chemotherapy may help predict chemotherapy response early, potentially allow for tailoring of treatment prior to surgery.
Lead author Dr Sheeba Irshad, Cancer Research UK Clinician Scientist from The School of Cancer & Pharmaceutical Sciences at King's College London, said:
"Chemotherapy resistance in aggressive early breast cancers is a major reason why cancer regrows after treatment, contributing significantly to people not surviving their disease. In order to find the right targets for drug developments, it’s important to have a deep understanding of the complex mechanisms that allow some cancer cells to resist treatment, then hide from our immune system to only re-emerge later when they’re harder to eradicate.
“Our work has identified several cell types that would be worth investigating further to understand how they are interacting with the resistant cancer cell and how we can tweak that for our benefit. I am excited to continue to investigate these findings further.”
Realising the potential of immunotherapy for breast cancer treatment
Professor Andrew Tutt, Director of the Breast Cancer Now Toby Robins Research Centre at the ICR and Director of the Breast Cancer Now Research Unit at King’s College London, said:
“Great strides have been made in harnessing immunotherapies to treat several types of cancer, but we need to do better to realise their potential for patients with breast cancer.
“This exciting work advances our understanding of the interaction between cancer cells and the immune system during treatment, and why existing treatments work well for some patients, but not others. I hope this research will help us to enhance the anti-cancer immune response in breast cancer, particularly for patients whose cancer has not responded well to chemotherapy.”
Dr Syed Haider, Bioinformatics Lead at the Breast Cancer Now’s Research Centre at the ICR, said:
“As new technologies enable affordable profiling of patient’s tumours over the course of treatment, we are able to gain a deeper understanding of the complexities of patient’s immune response.
“This study shows the power of integrating real-time information about a patient's tumour characteristics with dynamic changes in their circulating immune cells over the course of their treatment. Here, by combining an ensemble of techniques has given us unique insights into why chemotherapy is less effective for some patients, and may help us to identify patients who could benefit from immunotherapies."