Joint Integrated Pathology Unit
The Integrated Pathology Unit's pioneering research into diagnostics combines the power of digital pathology and artificial intelligence. These analytical approaches to cancer tissue-based research will streamline results.
The Integrated Pathology Unit (IPU) is a tissue-based laboratory. Our mission is to develop complex and highly quantitative approaches to tissue analysis (wet lab and in-silico) in the space of translational and clinical research.
This research is applicable in the context of clinical trials with potential adoption into the diagnostic setting.
The unit is a collaboration between the ICR and The Royal Marsden NHS Foundation Trust, along with other external collaborators.
How we research at this centre
The IPU is an operational and strategic advantage for the ICR and The Royal Marsden.
Operational
The research is championed by both institutions (supporting basic research, translational research and clinical/diagnostic research) requiring the same technologies, analyses of similar patient cohorts, and a reference laboratory quality. Creating this unit as a joint venture leads to consolidation of technology, human effort and IT resources, which, in turn, lead to laboratory efficiencies, cost-effectiveness and rapid translation.
Strategic
The IPU aims to develop excellence in digital pathology (DP) that supports research across the ICR and The Royal Marsden for the ultimate benefit of cancer patients. Developing a full offering of capacity and know-how in DP will also enable engagement with the pharmaceutical industry. Credible future bids for core infrastructure and research programmes are expected to benefit from a clear development of such capabilities.
Integrating research across the ICR and The Royal Marsden
We will coordinate with other programmes in the ICR and The Royal Marsden that are carrying out tissue-based analyses and AI quantification of digital images. We anticipate serving across academia, healthcare and industry.
This work is based on the PIs published experience, in collaborative research with other investigators, across the tissue-interrogation pathway. This includes:
- identification of biomarker clinical relevance (N Engl J Med. 2013 PMID: 23758232; J Natl Cancer Inst 2021; PMID: 32324860);
- clinical validation of molecular pathways (J Natl Cancer Inst. 2016; PMID: 27707838);
- key technical capacity to work with large clinical and clinical-trial cohorts, including tissue microarray construction (Br J Cancer. 2020; PMID: 32684627);
- single IHC analysis and RNA-ISH testing (Nat Rev Clin Oncol. 2018; PMID: 29358775);
- multiplex validations (Mol Oncol. 2020; PMID: 32671911; J Immunother Cancer 2020; PMID: 32414858); and
- diagnostic delivery (J Thorac Oncol. 2019; PMID: 30296485).
This is complemented with experience in open source and off-the-shelf use of digital pathology analyses.
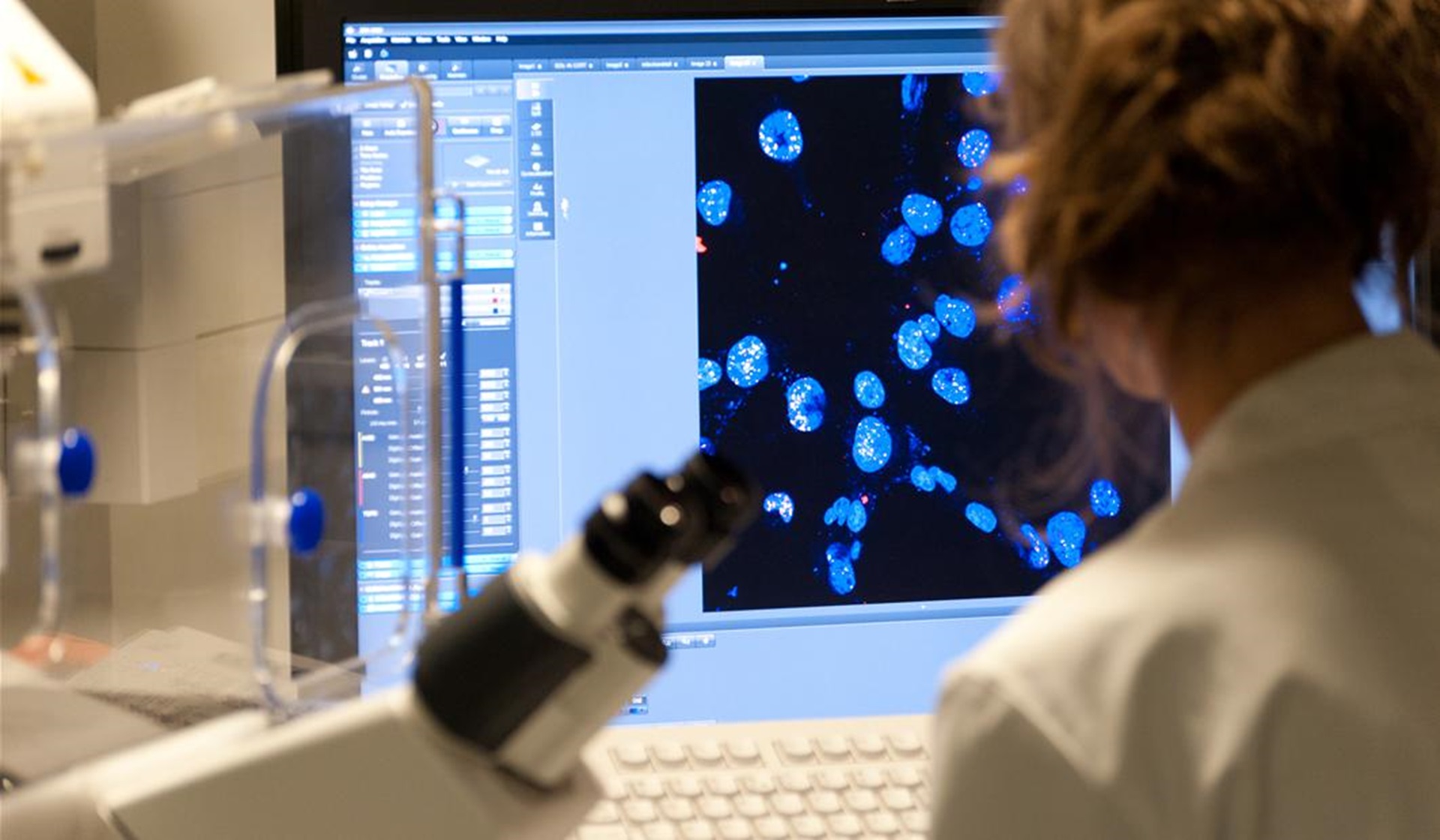
The newly created IPU will use state-of-the-art tissue-based profiling such as single-plex immunohistochemistry (IHC), RNA in situ hybridisation and IHC/IF multiplexing, together with multi-scan imaging and digital pathology / artificial intelligence (AI) biomarker quantitation.
These approaches will be applied to well-curated cancer sample cohorts (from routine diagnostics or from clinical trials) to:
- explore the clinical relevance of biomarkers and pathways
- identify the best quantitative delivery of biomarker analysis.
The IPU is recruiting a team of nearly 20 biologists and computer analysts. Our aim is to quantitatively define the spatial biology, tumour microenvironment and complexities of biomarker expression in order to identify their clinical applicability. The IPU is led by:
- Professor Manuel Salto-Tellez, Head of the IPU and Professor of Integrative Pathology at The Institute of Cancer Research, London
- Dr Katharina von Loga, Deputy Head of IPU and Consultant Molecular Pathologist at The Royal Marsden NHS Foundation Trust
- Dr Tom Lund, Scientific Lead of IPU and Senior Postdoctoral Research Fellow at The Royal Marsden NHS Foundation Trust
Personalised medicine (PM) in cancer is at the heart of molecular diagnostics and oncology treatment. PM is allowing some patients to live longer lives, and better lives. Unfortunately, the effect of these treatments is important but modest: most of these patients will develop resistance after a few months, coming back with disease that is often more genomically complex and clinically aggressive.
Furthermore, the current availability of biomarkers and associated treatments only applies to a minority of cancer patients. Better defining the molecular heterogeneity and evolutionary processes at the cellular level in tumours may lead to sequential or combination treatments for resistant cell populations that may be used to prevent or treat recurrence. Furthermore the promise of immuno-oncology is allowing some patients to enjoy long, sustainable survivals in some stages unthinkable to date; again, this is not generalisable and identifying robust predictors of immuno-oncological response has not been easy to date. Digital Pathology and Artificial Intelligence (DP/AI) has the capacity of improving this record by opening new translational research avenues and transforming the way we apply biomarkers in routine diagnostics.
Traditionally, the generation of research data for pathological or radiological images, or the application of first generation bioinformatics and biostatistical solutions to “big genomic data” has been the product of qualitative interpretation of results. AI holds the potential to describe a new reality from our phenotypic or genotypic information by obtaining extensive robust and quantitative results to establish links with clinical outcomes in an unprecedented manner and scale. This approach transforms the way we process and analyse pathological images, and link them in a meaningful way with clinical outcomes. In this regard, AI holds the potential of establishing a new cancer taxonomy by becoming the true facilitator of intergromics analysis.
How can a DP/AI systematic approach improve personalised medicine?
Artificial Intelligence (AI) is revolutionising cancer research. Indeed, AI is currently applied to drug design; genomic and image analysis; clinical decision-making; and population-based studies, in research and diagnostics. Tissue-based AI analysis by digital pathology (DP/AI) is arguably one of the most promising applications of AI to date at a number of different levels:
1. An improvement to genomic analysis.
The systematic annotation of tumour boundaries and the calculation of tumour content are everyday routine exercises in genomics laboratories, although it is well accepted that pathologists lack consistency, accuracy and reliability in this exercise. DP/AI algorithms bring consistency and accuracy to this analysis.
2. Quantitation of key oncology biomarkers.
The markers that are part of so-called therapeutic immunohistochemistry (ER, PR, Her2, Ki67, ALK, PDL1, etc) are scored at best in a semi-quantitative manner. Indeed, there always has been a clear understanding on the ground that many of these tests, widely applied by thousands of laboratories across the world, need a degree of consistency to fulfil their full potential.
3. A more accurate detector of important phenotypic features.
There is no question that some of the routine histopathological features of a cancer are still at the core of therapeutic decision-making. For instance, a histopathological assessment of a NSCLC between adenocarcinoma or squamous cell carcinoma is essential to decide on subsequent molecular analysis and treatment (gefitinib/erlotinib, crizotinib and pembrolizumab); or, for example, the pathological staging of a resected neoplasm (and, in particular the number of lymph nodes involved) is the single most important disease prognosticator and predictor of chemotherapy treatment. However, we know that there is a significant inter-observed and inter-departmental variation in these assessments. Recently, DP/AI approaches have been able to improve the detection of metastasis in lymph nodes, or the detection of basic pathological features in histopathology diagnosis. This opens the avenue for the histological assessment to be done more systematically and with better clinical outcomes via AI.
4. The powerful predictor of molecular features and gene expression signatures.
This is one of the key areas of development in translational research in tissue-based DP/AI. New algorithms are able to predict the presence and the general topography of mutations, in lung cancer and in other types of solid tumours; similar algorithms are able to predict more genome-wide information, such as the MSI-status; finally, new approaches to recapitulate the transcriptomic classification of cancers have also been achieved with this approach.
This is of significant relevance, not only in the fields of basic and translational research and the development of novel diagnostic tools, but also in the way we perform and analyse clinical trials. Indeed, part of the significant degree of attrition of cancer clinical trials when entering phase 3 is the disparity between observations made with cell lines in vitro (or animal in vivo) models and real-life patient outcomes. It is clear that the lack of adequate and realistic models to recapitulate cancer development is crucial, more significantly so when studying tumour micro-environment (TME). Thus, experimental research should move from cell lines and animal models of human disease directly to the “human models in situ”, something that is readily facilitated by DP/AI in clinical cases with high quality metadata.