Translational Immunotherapy Group
Professor Alan Melcher's group is looking at ways to activate the immune system to attack cancer using therapeutic viruses. These agents are already approved for clinical use and offer major potential benefits to further improve the promising field of immunotherapy.
Our group is interested in translational research linking laboratory findings to early clinical application, with a particular focus on therapeutic anti-cancer viruses.
Pre-Clinical Research
We are investigating local and systemic delivery of oncolytic viruses (OV) to tumours in mouse models, including in the brain. For example, we have shown that access of reovirus to tumours can be paradoxically enhanced by the presence of anti-viral neutralizing antibodies (NAb), which form complexes with reovirus for uptake, carriage and delivery to tumours by monocytes in the blood.
We are testing combination of systemic virotherapy (reovirus, herpes, vaccinia and maraba) with other immunomodulatory, clinical standard of care treatments (immune checkpoint blockade antibodies, targeted small molecules and radiotherapy).
We use murine models and human in vitro immune assays (including use of patient samples) to complement our translational trial data. This ensures we generate the most comprehensive pre-clinical dataset we can to optimize and guide future clinical development of novel OV and other immunotherapies.
Translational Trials
We perform biological endpoint, translational trials to address biological questions in patients. We have shown, using window-of-opportunity studies in patients planned for surgical resections, that intravenous reovirus successfully accesses tumours in patients with cancer in the liver or brain.
We are now developing further such studies combining OV with other immunomodulators, to ensure continuous, iterative translational research between laboratory and clinic to inform future trial development and benefit to patients.
Our group is interested in translational research linking laboratory findings to early clinical application, with a particular focus on therapeutic anti-cancer (‘oncolytic’) viruses (OV).
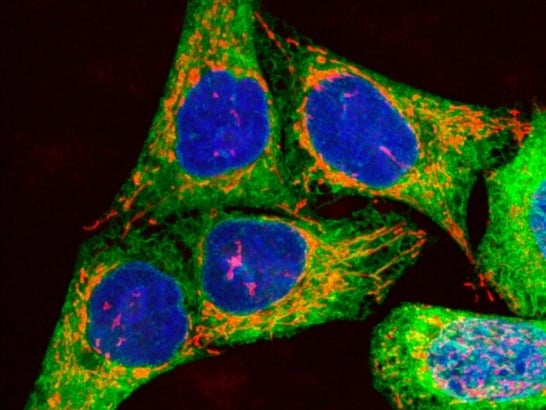
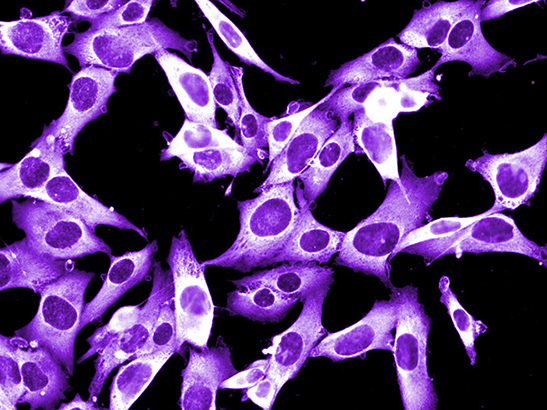
OV were initially developed as direct cytotoxic agents, to specifically infect, replicate within, and kill cancer cells. However, it has become increasingly clear that OV work more by stimulating an immune response against the tumour — i.e. they are a form of immunotherapy.
We work on a range of clinical grade viruses (reovirus, herpes, vaccinia and maraba), and have shown, using pre-clinical murine models, human in vitro immune assays and readouts from early, biological endpoint translational clinical trials in patients, that OV activate both innate and adaptive anti-tumour immunity.
Combining OV with other immune modulators, such as granulocyte-macrophage colony-stimulating factor, or checkpoint inhibitors can further enhance their efficacy. We are taking these pre-clinical findings back into the early clinical trial setting using an iterative ‘bench to bedside and back again’ approach.
While the only current clinically approved oncolytic virus (a herpes virus encoding GMCSF) is given by direct intratumoural injection, we believe that systemic administration of viruses is far more practical for widespread clinical application. We are therefore also testing intravenous OV delivery, in both the laboratory and the clinic, and have found, paradoxically, that anti-viral antibodies can actually enhance therapy by facilitating viral carriage by immune cells in the blood (specifically monocytes), to the tumour site.
We have confirmed OV access to tumours in patients following intravenous injection in patients with both colorectal cancer metastatic to the liver, and brain tumours (recurrent high grade gliomas or brain metastases). This has been done using ‘window of opportunity’ studies, giving OV prior to planned surgical resection of tumours as part of standard clinical care.
We are also testing incorporation of pre-clinically optimized systemic OV treatment with clinical standard of care treatments (immune checkpoint inhibition, radiotherapy or targeted small molecules), to ensure that our novel research findings are practically deliverable into the real clinical world, and to facilitate rapid benefits for patients with melanoma, head and neck, brain, and potentially other tumours.
Professor Alan Melcher
Group Leader:
Translational Immunotherapy, Breast Cancer Immunology
Professor Melcher is a clinician scientist studying how to activate the immune system to recognise and attack cancer. In particular, he works on oncolytic, anti-cancer viruses, which work mainly as a type of immunotherapy, and is a specialist in melanoma and head and neck cancer.
Researchers in this group
 .
.
Email: [email protected]
Location: Chelsea
Dr Irene Chong is a Clinician Scientist at The Institute of Cancer Research, London, and a Consultant Clinical Oncologist at The Royal Marsden NHS Foundation Trust.
Professor Alan Melcher's group have written 208 publications
Most recent new publication 3/2025
See all their publications .
.