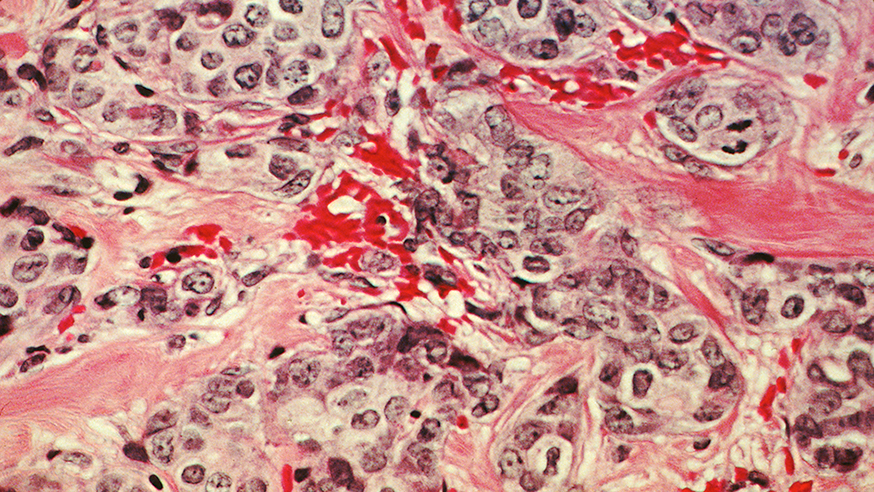
A histological slide of cancerous breast tissue. Source: National Cancer Institute
A new scan could help doctors to spot when women with breast cancer stop responding to targeted drugs.
Researchers at The Institute of Cancer Research, London, developed a ‘molecular tracker’, which highlights a protein that indicates drug resistance during PET scans.
In studies in mice, the tracker lit up pockets of tumours which contained high levels of a protein called HER3, which is linked to resistance to cancer drugs called HSP90 inhibitors.
The research, published in Clinical Cancer Research, could guide the use of Hsp90 inhibitors to deliver personalised treatment plans for some patients with breast cancer.
As part of our research into hormone receptor-positive breast cancer we are developing a new breast cancer modelling facility which will let us fast-track new treatments to the patients who need them now.
HER3 and resistance to targeted treatments
Studies with Hsp90 inhibitors, which were discovered at the ICR, have identified these inhibitors as promising drugs for breast and prostate cancer if used in combination with other treatments.
But certain breast cancer cells can develop HER3-mediated resistance to Hsp90 inhibitors.
Currently, HER3 levels are measured using tissue samples taken from a patient’s tumours. These are uncomfortable to collect and may not accurately reflect HER3 activity across the tumour, or in other tumours from the patient.
Scans measure antibody-mimicking biomarker
Dr Gabriela Kramer-Marek, leader of the Preclinical Molecular Imaging team at the ICR, led the research to develop the molecular tracker, which attaches to HER3 in cancer cells.
The tracker was developed using affibody molecules – small proteins engineered to act like antibodies to recognise and bind to target molecules in the body.
PET scans of mice with breast cancer showed the radioactively tagged biomarker could identify HER3 in cancer cells.
The scans also indicated increases in HER3 activity in mice treated with Hsp90 inhibitor drugs, compared with untreated mice, demonstrating the development of resistance to treatment.
A valuable tool to deliver personalised treatments
The study was funded by the ICR and the Cancer Research UK-Cancer Imaging Centre at the ICR and The Royal Marsden NHS Foundation Trust, with support from AffibodyAB.
Lead author Dr Gabriela Kramer-Marek said: “HER3 is a key player in the lack of response to targeted therapies used to treat breast cancer. Our research shows PET scans of radio-tagged affibody molecules can measure changes in HER3 levels in breast cancer.
“We believe that HER3 PET imaging could be an important way to measure changes to HER3 resulting from resistance to targeted treatments, and become a valuable tool to deliver personalised treatments for patients with cancer.”

 .
.