New adaptive radiotherapy technique for head and neck cancer can deliver a more robust treatment plan in a shorter timeframe on the MR Linac, compared with the current method used by most radiotherapy centres.
The new approach, known as ‘ATS-Lite’, achieved 99.9 per cent accurate radiotherapy delivery in a tolerable timeframe, making it more comfortable for patients
The research, led by researchers at The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust and funded by Cancer Research UK, could lead to increased use of the MR Linac for head and neck cancer globally, in a simpler and quicker way.
The study was published in the journal Clinical and Translational Radiation Oncology.
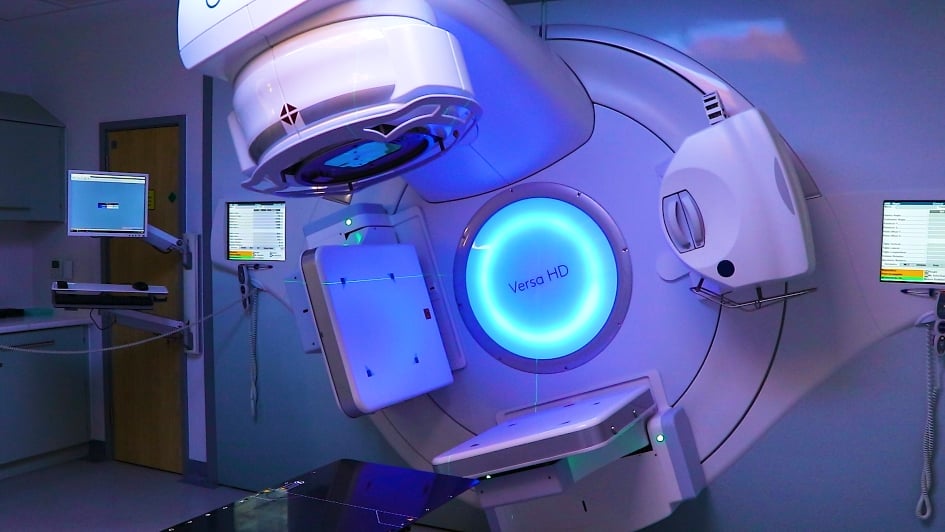
The aim of this study was to report the result of the novel technique, treating the first two patients with head and neck cancer on the MR Linac – the first technology to simultaneously generate magnetic resonance images and deliver X-rays, precisely locating and visualising tumours and surrounding organs at risk while delivering radiation.
The ICR and The Royal Marsden were the first institutions in the UK to install an MR Linac machine, which allows radiotherapy to be adjusted in real time. The installation of the MR Linac was made possible by a £10m grant from the Medical Research Council to the ICR, with additional support from The Royal Marsden Cancer Charity.
Greater accuracy
The shape and position of a tumour relative to nearby healthy tissue changes over the course of treatment and often during a single treatment session, which is why clinicians use ‘adaptive’ radiotherapy – enabling greater treatment accuracy.
During adaptive radiotherapy, daily updated images are acquired right before treatment and the radiotherapy delivery plan is adapted accordingly. This helps account for changes in the patient’s or tumour’s anatomy, delivering radiation accurately to avoid surrounding organs at risk.
The two adaptive radiotherapy treatment options on the MR Linac are adapt-to-position (ATP) and adapt-to-shape (ATS). With the ATP approach, only the patient’s position is updated, while ATS accounts for anatomical changes.
ATP lacks accuracy, often requiring off-line replan while full ATS requires the patient to remain on the treatment table, immobilised in a tightly fitting mask for long periods of time, making it unreasonable for daily use.
Adaptive radiotherapy
But researchers have identified a new strategy – ATS-Lite, a ‘half-way’ approach that provides adaptive radiotherapy without requiring daily clinician presence to perform target and organ-at-risk recontouring.
ATS-Lite makes this possible by accounting for external contour changes which are commonly seen in head and neck cancer patients due to weight loss or tumour response. Using the ATS-Lite software, the external contours can be accurately generated in an automated way.
Researchers compared how the ATS-Lite approach performed against what would have been generated using ATP. They delivered and analysed 53 radiotherapy doses. ATS-Lite passed 99.9 per cent of mandatory dose constraints, while the ATP technique failed 7.6 per cent of the dose constraints – meaning it had a higher rate of plan ‘failure’.
The average treatment duration for the two patients using the ATS-Lite approach on the MR Linac was 40 mins 9 s and 32 mins 14 s, respectively. In comparison, the go-to ATP approach takes an average time of 46 mins, while the full ATS which is considered gold-standard, remains unfeasible – no centre has been able to treat head and neck cancer using ‘full ‘ATS yet, as the treatment time would be over an hour.
Faster, kinder treatment
The main advantage of ATS-Lite compared with ATP is the robustness of the generated plan. Because ATP has a higher rate of plan failure, patients have to be repositioned more frequently, which significantly adds on to the treatment time. Full ATS requires a daily clinician presence on the machine to recontour, which is why it also takes longer.
ATS-Lite is a ‘half-way’ approach that takes into account the contour change and any additional benefit from ‘full’ ATS would be minimal. For this reason, researchers believe that ATS-Lite is the way forward to treat head and neck cancer patients on the MR Linac.
Study leader Dr Kee Howe Wong, Consultant Clinical Oncologist at The Royal Marsden NHS Foundation Trust, said:
“Adaptive radiotherapy allows for flexibility to adapt the radiotherapy treatment plan to the patients’ anatomy in daily treatment session. ATS-Lite is a new and improved approach and, though we’re at an early stage, we have seen great results so far, with patients responding very well to the treatment.
“We now plan to further test, utilise and develop this approach in the coming months. This includes assessing advanced imaging on the MR Linac to guide whether we can safely decrease the radiotherapy dose, which could help to reduce side effects, or escalate treatment if the patient isn’t responding sufficiently to the treatment. We are also working with our international colleagues within the MR Linac consortium to gather data to develop evidence-based treatment.”
Increase cure rates
Study author Professor Kevin Harrington, Head of the Division of Radiotherapy and Imaging at The Institute of Cancer Research, London and Consultant Oncologist at The Royal Marsden NHS Foundation Trust, said:
“We have come up with a new method to deliver radiation to head and neck tumours in a tolerable timeframe using the MR Linac, making treatment sessions shorter and more comfortable for patients.
“The ATS-Lite approach will help us perform daily adaptive radiotherapy in a simpler and more efficient way, enabling us to move on from a ‘one size fits all’ approach and helping to increase cure rates and reduce side effects.
“A few hospitals across the MR Linac Consortium have already started adopting the approach, which we hope will benefit many head and neck cancer patients while also saving time and resources, as it removes the need for a clinician to be present during radiotherapy delivery.”
Retired firefighter Andy Johnstone, aged 65 from Fetcham, Surrey, was diagnosed with head and neck cancer at his local hospital in May 2021. He was referred to The Royal Marsden and was one of the first patients to be treated with this new MR Linac technique. He said:
“In 2020, I developed a sore throat and, the following year, I noticed it felt like there was something there when I swallowed, so I decided to get checked out. It turned out I had a very large tumour which was in my tongue, tonsils, throat, and some lymph nodes. A week after my diagnosis, I had an appointment with Dr Wong at The Royal Marsden who said he could help me and asked if I was claustrophobic. I said no, having been a firefighter for 32 years. He said I could have this experimental new form of radiotherapy, which I thought sounded brilliant. I was up for doing anything that might help, and it was good to know I was supporting research that could help others too.
“I was treated in the MR Linc five days a week, for six weeks. The machine is quite a small space, but the hospital’s staff made me feel as comfortable as possible. They regularly spoke to me through the system, played music of my choice and, when my treatment finished, they were all there to give me a round of applause. My birthday was in August and, as a way of saying thanks, I set up a fundraiser via Facebook for The Royal Marsden Cancer Charity and raised over £1,000.
“I had a follow-up scan in December which showed that there was no sign of cancer. I’m so glad I had this treatment which, according to my healthcare team, probably saved my life. While my taste has been affected – I can’t eat spicy foods or drink red wine – I’m now doing really well, walking 10,000 steps a day, doing some decorating for friends and family, and spending time with my wife, three children, five grandchildren and twin great-grandsons.”
An exciting new approach
Michelle Mitchell, Cancer Research UK’s Chief Executive, said:
“Cancer Research UK was instrumental in the development of radiotherapy, and we’ve been refining, improving and innovating the treatment for nearly a century.
“Each year radiotherapy benefits over 130,000 patients in the UK, but the treatment can be uncomfortable, so reducing the time a patient spends exposed to radiation but still ensuring the treatment is as accurate and effective as possible, is key.
“Adapting radiotherapy based on the patient’s anatomy and tumour is an exciting new approach that could make radiotherapy work better for patients and make the unpleasant experience of radiotherapy more comfortable.”

 .
.
 .
.