Pancreatic cancers recycle resources to fuel their survival and growth, opening up the possibility of new treatments aimed at stopping them from doing so, scientists report.
New findings show that pancreatic cancers make use of a key ‘recycler’ protein to keep pace with their constant demand for oxygen and energy, as they grow and spread.
Blocking the recycler could suffocate pancreatic cancer cells by starving them of oxygen and energy – and the researchers now plan to create new drugs aimed at suffocating tumours.
The new study is the first to investigate the role in pancreatic cancer of ‘deubiquitylating enzymes’ (DUBs) – which stop other proteins from being ‘binned’ by the body so they can be recycled instead.
USP25, a key 'recycler' protein
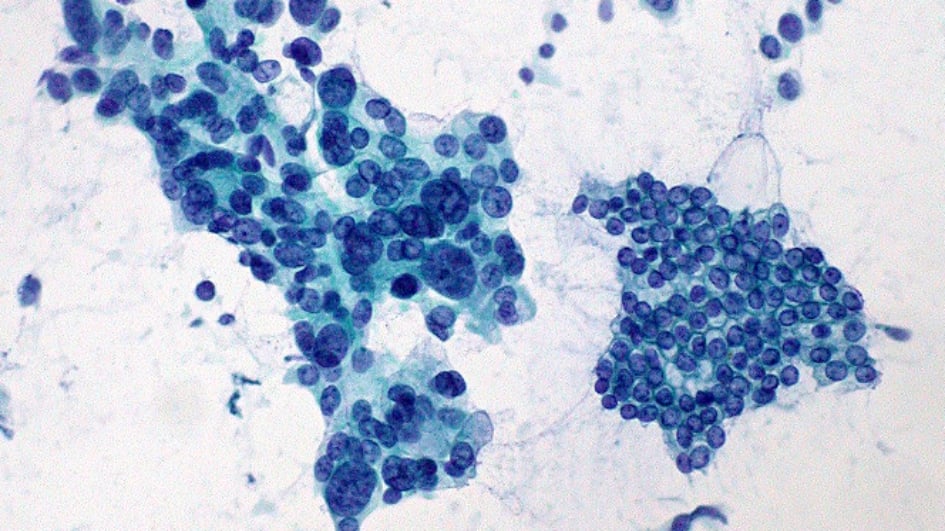
The team, led by scientists at The Institute of Cancer Research, London, used protein analysis techniques in mice and in ‘mini-tumours’ grown in dishes from patient tissue to explore the role of DUBs in pancreatic ductal adenocarcinoma (PDAC).
They identified a DUB called USP25 as a key ‘recycler’ protein which supported the survival and growth of cancer cells.
The research, published in Nature Communications, was funded by Cancer Research UK, Wellcome, Breast Cancer Now and two UKRI councils – the Engineering and Physical Sciences Research Council and the Medical Research Council.
Pancreatic tumours are known to have low oxygen ‘micro-environments’. This is because the rapid growth of pancreatic cancer often outstrips the oxygen supply, which cancer cells need to survive and grow.
Researchers found that USP25 can regulate a protein known as HIF-1a to help pancreatic cancer cells adapt to low oxygen levels in the tumour. USP25 does this by preventing HIF-1a from being ‘binned’, so it can form new blood vessels to supply the cancer with oxygenated blood.
Cancer cells starved of oxygen
Scientists showed that genetically deleting USP25, or blocking it using drugs, meant mini-tumours were unable to grow, as they were starved of oxygen.
Researchers believe that by acting as a ‘recycler’ protein, USP25 can reverse the protein modifications on HIF-1a that destine it to be degraded by the body, stabilising HIF-1a and allowing it to continue supplying oxygen and nutrients to cancer cells. In this way, USP25 plays a role in helping pancreatic cancer grow and spread.
Researchers believe the mechanism may also be important for other low-oxygen tumour types, such as breast cancer, and plan to explore it further.
Next, researchers will seek to design USP25 inhibitors and ultimately to assess the new approach to treatment in patients with pancreatic cancer. They are also planning to investigate the role of other druggable DUBs in pancreatic cancer.
The Institute of Cancer Research (ICR) launched its new Centre for Protein Degradation last month, where scientists will aim to exploit the normal waste disposal system in cells to create new forms of cancer treatment. The ultimate aim of the centre is to lead to new treatments for patients with currently un-druggable, hard-to-treat cancers.
The new Centre for Protein Degradation was made possible by a £9 million donation to The Institute of Cancer Research, London – which is a charity as well as a world-leading cancer research institute.
More about the Centre for Protein Degradation
A new approach for a hard-to-treat cancer
Professor Axel Behrens, Scientific Director of the Cancer Research UK Convergence Science Centre at The Institute of Cancer Research, London, and Imperial College London, said:
“Our findings show that pancreatic cancers recycle proteins within cells to keep pace with their demand for oxygen and energy. By stopping other proteins from being degraded by the body, the recycler protein USP25 can help provide oxygen and nutrients to cancer cells, fuelling their growth.
“If we can create drugs to stop USP25 from carrying out its recycling function, we may be able to suffocate cancer cells by starving them of oxygen and energy. We hope to eventually be able to test this new approach in people with pancreatic cancer – a particularly hard-to-treat and deadly form of the disease.”
Professor Kristian Helin, Chief Executive of The Institute of Cancer Research, London, said:
“This study sets out an exciting scientific discovery – that pancreatic cancers need to recycle resources to stay alive and continue to grow.. Pancreatic cancer is extremely aggressive and hard to treat, and we need brand new, highly innovative approaches if we are going to crack it. I very much look forward to the next stages of this research, as our scientists aim to create potential new treatments for pancreatic tumours.”
Dr Megan Dowie, MRC Head of Molecular and Cellular Medicine said:
“This study is an excellent example of how multi-modal research can look at important challenges in human health and disease.
“UKRI is committed to improving our integrated understanding of disease and we look forward to seeing how next steps in this work can further impact our understanding and treatment of pancreatic cancer.”

 .
.