Repurposing existing cancer drugs to exploit a genetic weakness
July 2023
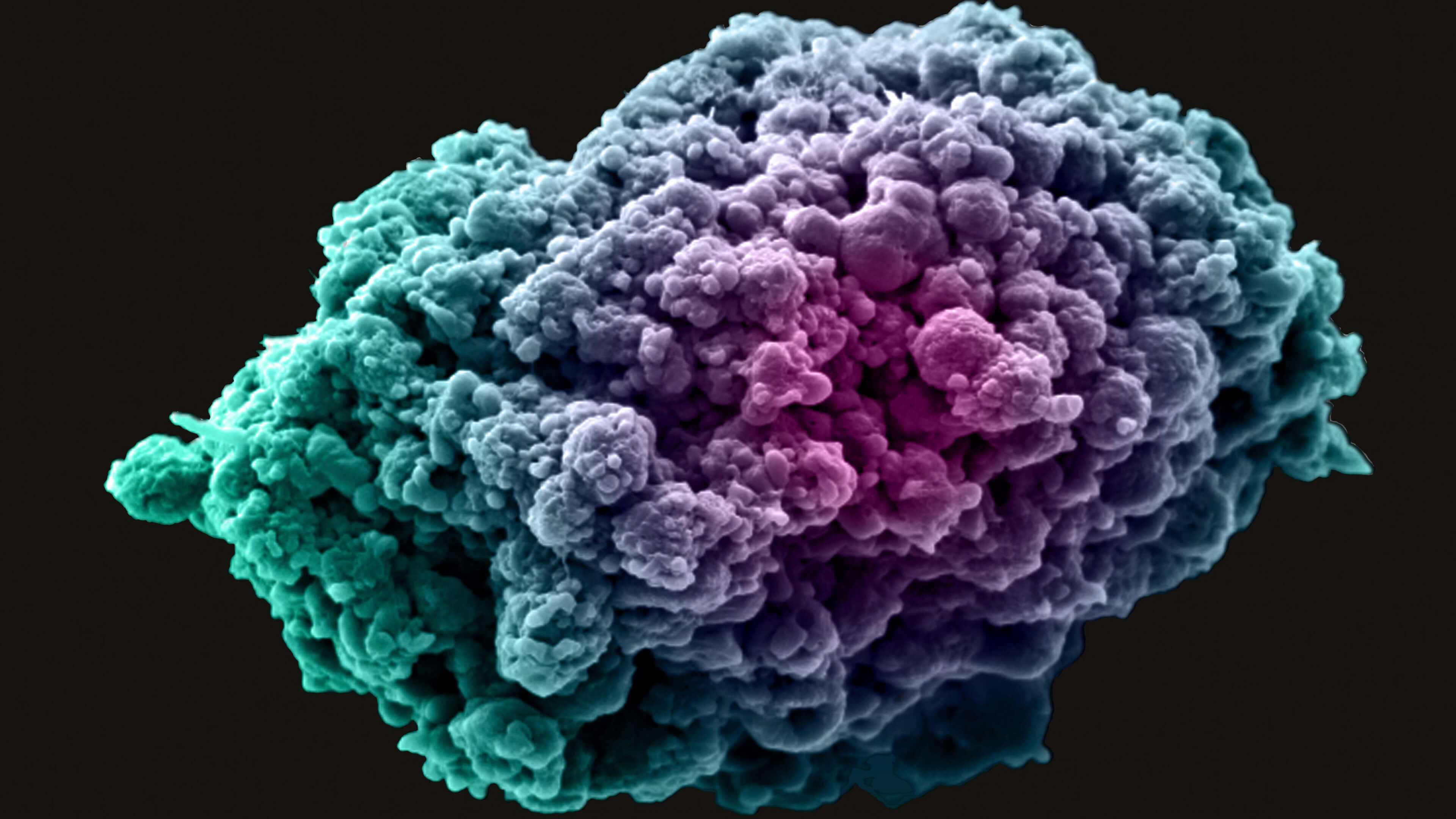
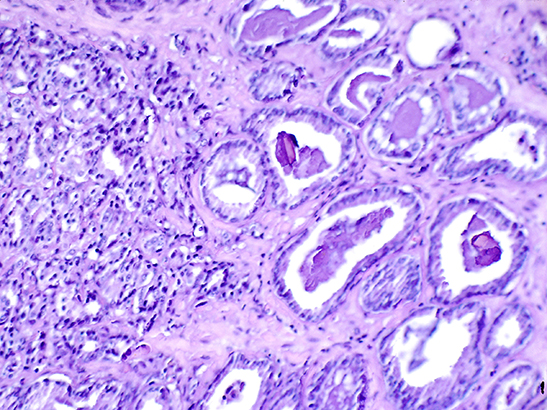
Dr Rachael Natrajan, Leader of the Functional Genomics Group at the ICR, recently led investigative work on a gene called SF3B1, which plays a part in processing the genetic information used to build proteins. The gene has been linked to several types of cancer, including some ER+ breast cancers and certain types of leukaemia and melanoma.
In the first stage of the study, the researchers, working in the Breast Cancer Now Toby Robins Research Centre at the ICR, showed that cells with an altered SF3B1 gene lack a protein called CINP. They found that they could exploit this using drugs called PARP inhibitors to hamper the cells’ ability to copy their DNA accurately, thereby preventing cancer growth. In the second stage, the team assessed the efficacy of 80 of these drugs against cancer cells with an altered SF3B1 gene, finding that the treatments reduced the cells’ ability to survive.
The ICR has been involved in the development of PARP inhibitor drugs, which include olaparib, for many years, and these medications are already used to treat some breast, ovarian and prostate cancer patients who have inherited an altered BRCA1 or BRCA2 gene. This latest research suggests that PARP inhibitors could also be used to treat the thousands of patients with mutations in the SF3B1 gene, potentially transforming the treatment of multiple cancer types.
Targeting blood cells that cancer uses to promote its growth
October 2023
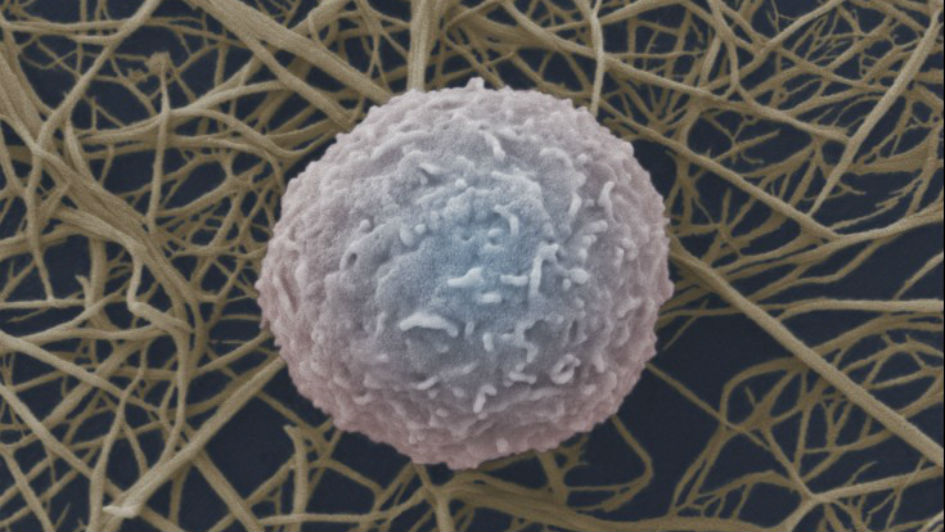
Researchers at the ICR co-led a recent study showing that it is possible to reverse drug resistance and slow tumour progression in prostate cancer by targeting myeloid white blood cells. Tumours can ‘hijack’ these cells to help fuel their growth, progression and resistance to treatment.
Professor Johann De Bono, Regius Professor of Cancer Research at the ICR, led the study, which could lead to an entirely new way of treating prostate cancer. Based on their knowledge that myeloid cells are elevated in patients with more aggressive tumours, the scientists had theorised that the cells contributed to treatment resistance. For the study, they recruited patients with advanced prostate cancer and gave them an experimental drug called AZD5069 alongside the hormone therapy commonly used to treat the disease. The addition of AZD5069, which blocks tumour cells from recruiting myeloid cells, led to increased tumour shrinkage and decreased circulating levels of prostate specific antigen (PSA), a marker of the disease.
This study was the first to prove that preventing myeloid cell recruitment, which AZD5069 does by blocking a receptor on the myeloid cells, has anti-tumour activity in humans with prostate cancer. The next step is to test this treatment approach in clinical trials involving more patients.Using AI to improve the accuracy of diagnosis
November 2023
Collaborative work from the ICR and its hospital partner, The Royal Marsden, has shown that artificial intelligence (AI) has the potential to benefit thousands of cancer patients each year by improving the accuracy of diagnosis. Professor Christina Messiou, Consultant Radiologist at The Royal Marsden and Professor in Imaging for Personalised Oncology at the ICR, led the study, in which a new AI algorithm was revealed to be around twice as accurate as a biopsy in grading the aggressiveness of a rare soft tissue cancer called retroperitoneal sarcoma.
The researchers created the algorithm using CT scans from 170 people with this disease, all of whom were treated at The Royal Marsden. When they tested it on nearly 90 patients based in Europe and the US, they found that the model accurately determined the likely aggressiveness of 82 per cent of the tumours analysed. This was much higher than the 44 per cent correctly graded using a biopsy. The model was also able to differentiate between the two most common forms of retroperitoneal sarcoma in 84 per cent of cases, while radiologists were only able to do this in 35 per cent of the sarcomas tested. By improving the accuracy of diagnosis, this technique could improve the management of the disease, leading to better outcomes for patients.
Identifying a potential new drug target in acute myeloid leukaemia
November 2024
.jpg?sfvrsn=21a64ae3_1)
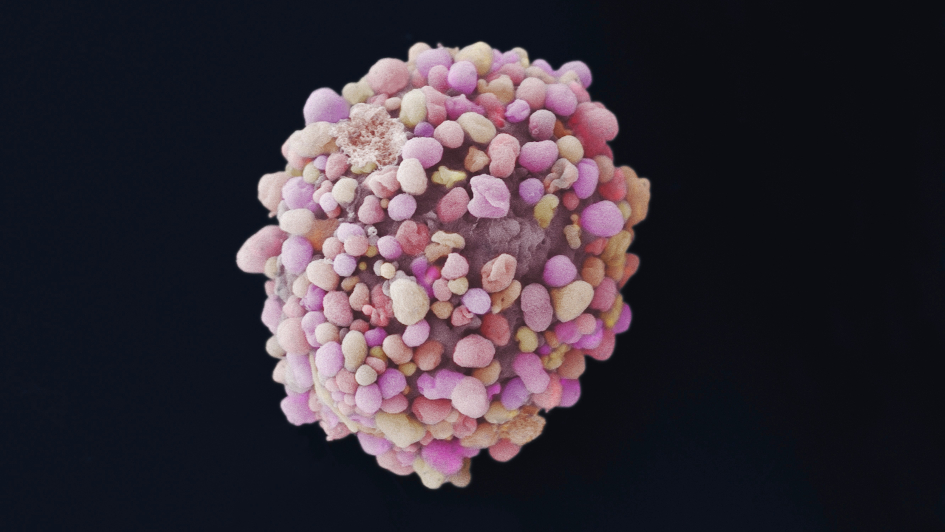
A team of researchers led by Professor Kristian Helin, Chief Executive and Professor of Epigenetics and Cancer at the ICR, set out to identify new vulnerabilities in acute myeloid leukaemia (AML), an aggressive form of blood cancer with a low survival rate. The scientists decided to focus on MLL-rearranged AML – a type of the disease driven by a common mutation that affects blood cell production.
They used a versatile tool called CRISPR interference (CRISPRi) to screen 1,046 genes associated with regulating the packaged DNA in these cancer cells. The aim was to identify genes involved in packaging DNA that was also required for sustaining the proliferation of AML cells. This led to the identification of an alternative form of the nucleosome remodelling factor (NURF) that plays an important part in regulating gene expression.
The scientists showed that the alternative NURF complex comprises proteins called BPTF, SMARCA5 and BAP18, and that BPTF is essential for AML cells to grow and multiply. Overall, this protein complex promotes the survival of AML, meaning drugs that target it could potentially control or eliminate the disease. This important work has opened the door to a new therapeutic strategy that might lead to much-needed new treatments for AML.
Overcoming a longstanding technical challenge in drug discovery
April 2024
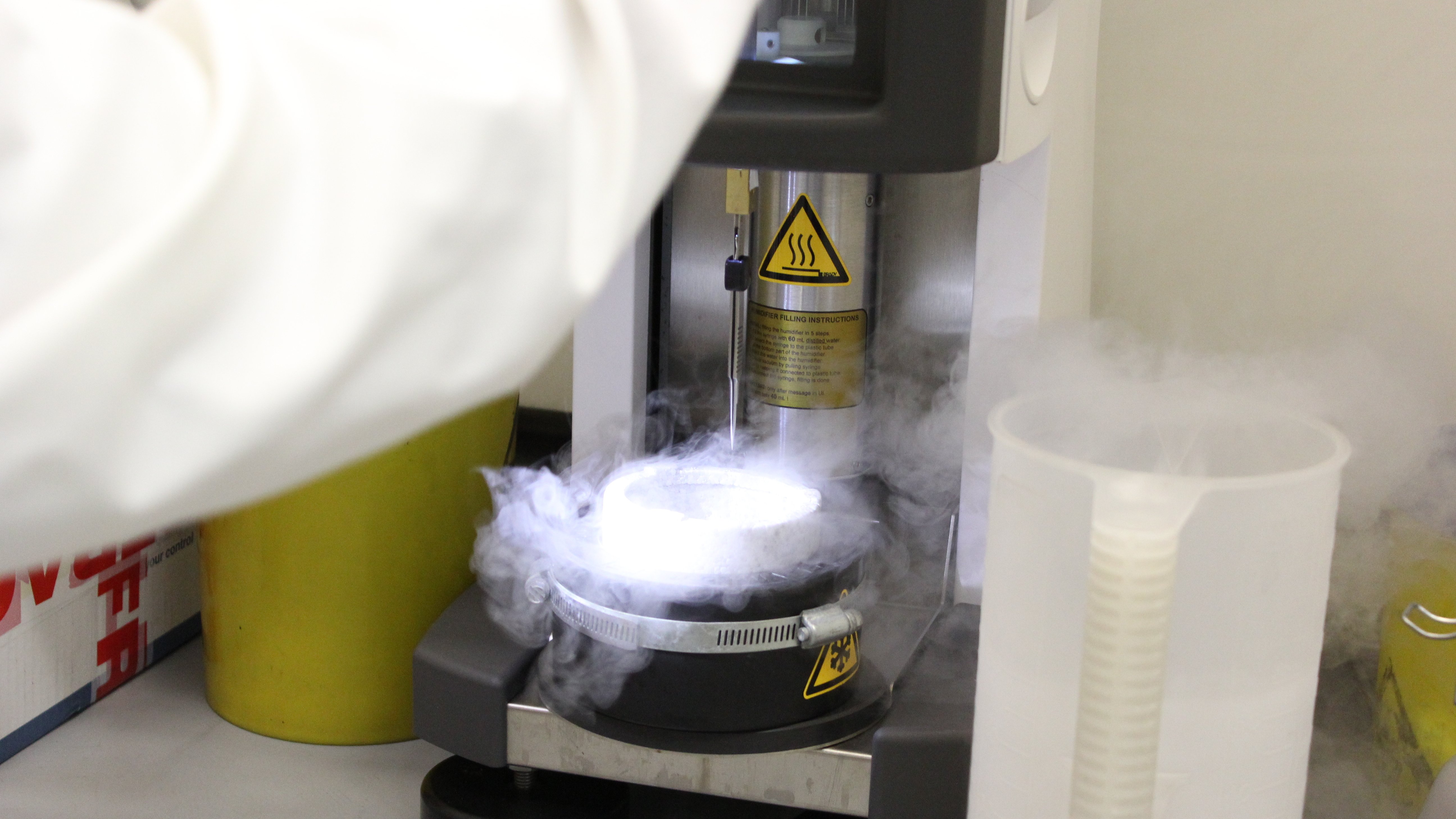
The structural biology community is likely to benefit from a groundbreaking methodological advance made by scientists at the ICR. The team developed a new cryogenic electron microscopy (cryo-EM) workflow that provided higher-resolution images in a shorter timeframe. The resulting images will help scientists determine the structure and interactions of protein complexes more accurately.
Cryo-EM can reveal the detailed structure of biological molecules by rapidly freezing samples to below -150° before passing a beam of electrons through them to collect images from different angles. However, both the resolution of the images and the time it takes to produce them can limit the use of this technique.
In the study, led by Dr Basil Greber, Structural Biology of DNA Repair Complexes Group Leader at the ICR, the researchers developed an improved cryo-EM workflow involving two stages. They began by performing rapid screening using a less costly and more readily available cryo-EM instrument to select the specimens with high potential. For these only, they then used a cold field emission gun to obtain higher resolution images. This approach allowed the team to achieve exceptional images at a resolution that had only ever been achieved for one protein complex of a similar size before. It also made it possible for the team to determine more than 12 structures per day – an impressively high number.
In this case, the researchers used their new technique to determine 16 detailed structures of a protein complex known as CAK, which has shown promise as a target for cancer drugs. However, the team believes that scientists in other labs will be able to apply the new methodology to drug discovery, meaning it could support the design of multiple next-generation therapeutics.
Finding a new treatment approach for a cancer of unmet need
April 2024
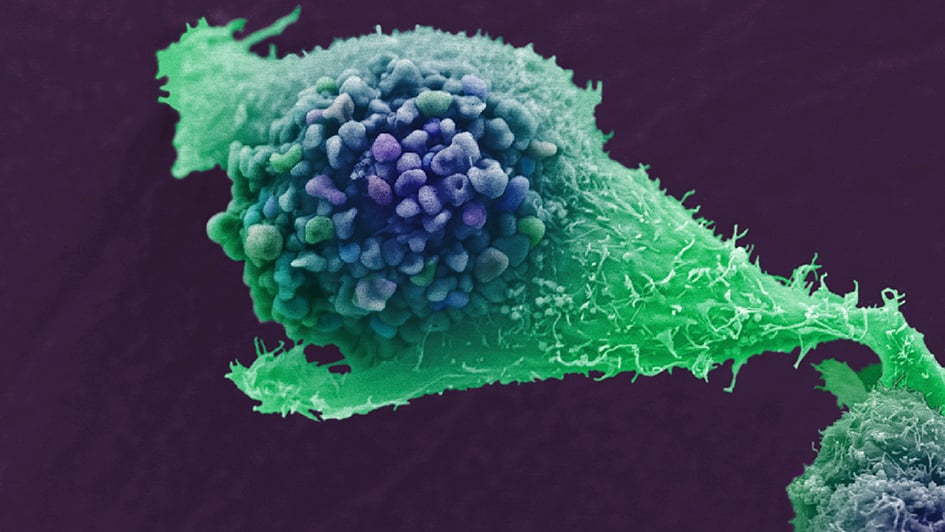
Groundbreaking work co-led by researchers at the ICR has demonstrated the feasibility of a new treatment approach for acute myeloid leukaemia (AML), an aggressive type of blood cancer for which there are currently limited treatment options.
The team, led by Professor Kamil Kranc, Professor of Haemato-Oncology at the ICR, investigated enzymes called prolyl hydroxylases (PHDs), which promote aggressive AML by targeting proteins called HIF proteins for destruction. PHDs become less active when oxygen levels are low, and the scientists had previously used this to show that these conditions result in increased levels of HIF.
In this study, the team successfully used genetic modification to inactivate PHDs in mice and used existing anaemia drugs to do the same in patient samples. In both cases, PHD inactivation led to higher HIF levels and stopped leukaemia from starting or progressing. The researchers then built on these findings to develop a new first-in-class PHD inhibitor called IOX5, which blocked AML progression by selectively inhibiting PHDs. They were then able to further increase the anti-cancer effect of IOX5 by combining it with an existing leukaemia drug called venetoclax.
Gaining an important insight into the mechanisms promoting breast cancer recurrence
March 2024
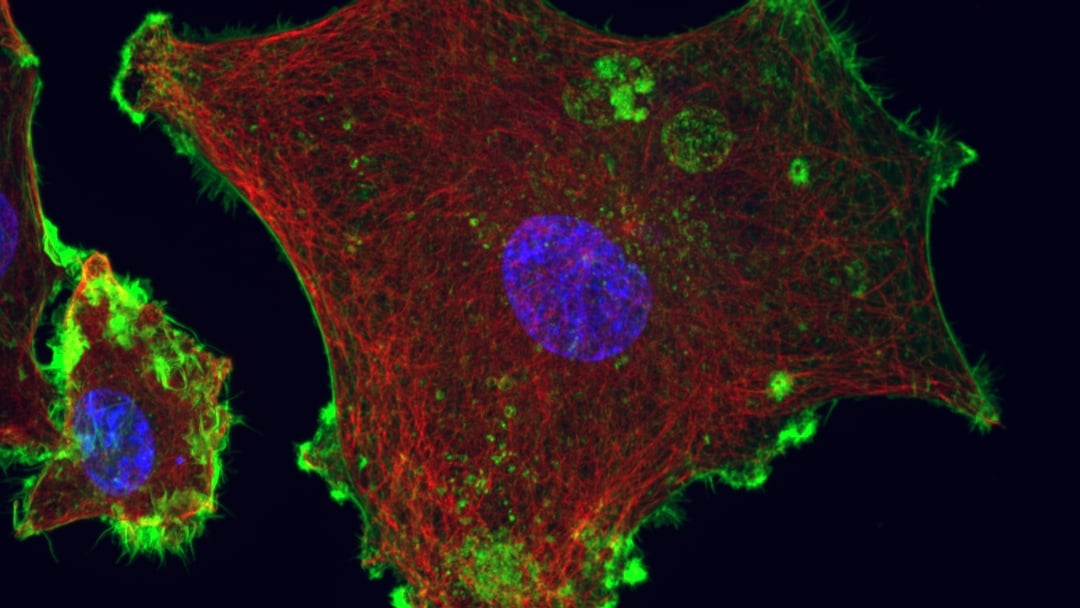
Early-stage research carried out by scientists in the Breast Cancer Research Division at the ICR has uncovered the role of epigenetic changes – which alter how genes work without changing the body’s DNA code – in breast cancer recurrence. The group, led by Professor Luca Magnani, Professor of Epigenetic Plasticity at the ICR, found that specific changes to proteins in chromatin, which is the condensed structure of DNA in cells, can cause oestrogen receptor positive (ER+) breast cancer cells to ‘hibernate’, allowing them to survive treatment. They can then ‘wake up’ years later, causing a relapse that is difficult to treat.
The work, which was started at Imperial College London and completed in the Breast Cancer Now Toby Robins Research Centre at the ICR, showed that hormone therapy could trigger these epigenetic changes. By targeting an enzyme called G9a, the scientists were able to block the changes, destroying cells that had already become dormant and preventing other cells from entering this state. This work could support the development of new treatments that prevent breast cancer from recurring following initial treatment for the disease.
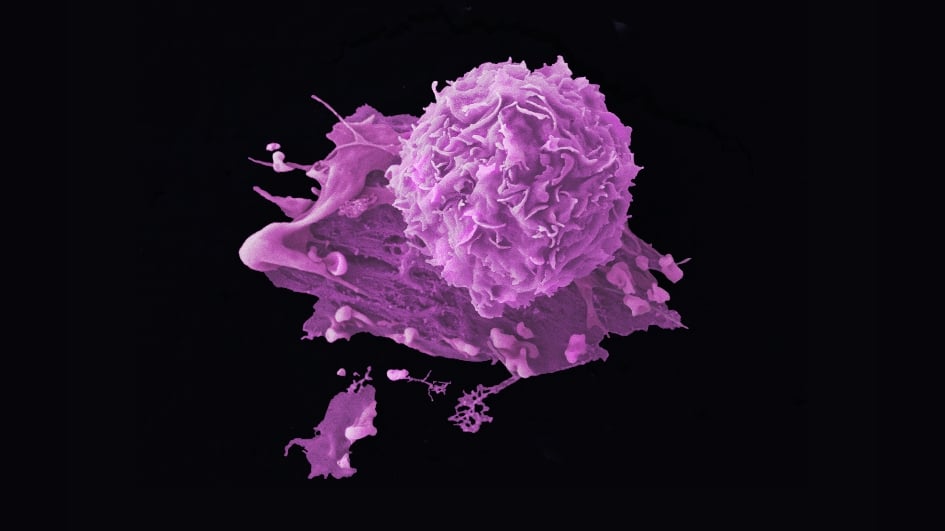
Using the cell’s own machinery to destroy a key cancer protein
A new and innovative technology has successfully been used by ICR scientists to destroy RIPK1, a protein that is crucial for breast cancer cells to remain undetected and survive. Through a process known as targeted protein degradation, the technology – called proteolysis targeting chimera (PROTAC) – eliminates RIPK1, which triggers a particular form of cell death that switches on the immune system and makes it alert to the cancer. Once mobilised, the immune system can destroy any remaining cancer cells that have evaded treatment or become resistant to it.
For the pre-clinical study, which was carried out using mouse models, scientists in the Breast Cancer Now Toby Robins Research Centre at the ICR, led by Professor Pascal Meier, collaborated with colleagues at the ICR’s Centre for Cancer Drug Discovery and Centre for Protein Degradation. Their new approach to killing breast cancer cells, which effectively trains the immune system to recognise them, could provide patients with longer lasting protection from the disease. This approach may be effective for a range of cancer types, including triple negative breast cancer, which is known for its high recurrence rate and for being particularly difficult to treat.
Reducing the likelihood of disease recurrence, and the associated anxiety, could significantly improve quality of life for people whose initial treatment proves successful.
Making a ‘practice-changing’ discovery that may spare patients from unnecessary treatment
May 2024

Professor Chris Parker, Professor of Prostate Oncology at the ICR and Consultant Clinical Oncologist at The Royal Marsden, was chief investigator on the phase III RADICALS-HD trial, which produced findings that might change the standard of care in a certain group of prostate cancer patients.
In the trial, the scientists assessed the value of hormone therapy when given alongside radiotherapy following surgery to remove the prostate. A total of 1,480 people with low-risk prostate cancer were randomly assigned to two groups – the first received only postoperative radiotherapy and the second received hormone therapy in addition.
After 10 years, the team found that 79 per cent of the people in the first group had survived without their cancer spreading, compared with 80 per cent of those in the second group. This small difference, which could be due merely to chance, demonstrates that hormone therapy provides no significant benefit for this patient group. This means that patients with a lower chance of their cancer returning could be spared from hormone therapy, which can cause a range of side effects, including erectile dysfunction and loss of muscle mass and bone density.
Identifying previously unknown cancer drivers that could aid precision
November 2024
A large-scale analysis of whole-genome sequencing data revealed 330 unique genes likely to have a role in driving cancer, 74 of which had not previously been identified. The study, led by Professor Richard Houlston, Head of the Division of Genetics and Epidemiology at the ICR, used data from 10,478 patients spanning 35 cancer types. All these individuals were participating in the 100,000 Genomes Project, a UK initiative to provide an information bank that could help researchers study the role of human genes in various diseases.
The researchers looked for common associations between mutations and cancer types to help them identify possible culprit genes. They were able to detect up to 80 per cent of the known driver genes, confirming the validity of their approach. In addition, they identified new cancer driver genes in several cancer types, including uterine, bladder and colorectal.
Importantly, the researchers believe that about 55 per cent of patients’ tumours are likely to harbour a mutation that could predict their response to certain treatments. In addition, they estimate that 15 per cent of patients may be eligible for a currently approved therapy targeting known oncogenes, which include HER2 in breast cancer and KRAS in multiple cancer types.
Using the information from this study and similar work to inform diagnostic panels could, therefore, help clinicians determine the optimal treatments for patients based on the genetics of their cancer.