The Institute of Cancer Research, London, strongly welcomes the decision by NICE to recommend the targeted breast cancer drug, capivasertib, in combination with fulvestrant, for treating the most common type of advanced breast cancer with specific biomarker alterations (PIK3CA, AKT1 or PTEN).
The judgement makes this new drug combination available for 1,100 patients a year on the NHS in England and Wales with hormone receptor (HR) positive, human epidermal growth factor receptor 2 (HER-2) negative breast cancer, which has advanced or spread following treatment.
The new drug is suitable for patients' tumours with mutations or alterations in the PIK3CA, AKT1 or PTEN genes – found in approximately half of patients with this form of breast cancer. The treatment could eventually benefit around 3,000 patients a year. The treatment could eventually benefit around 3,000 patients a year.
The recommendation follows the approval of capivasertib by the Medicines & Healthcare products Regulatory Agency (MHRA) in July 2024.
A first-in-class drug
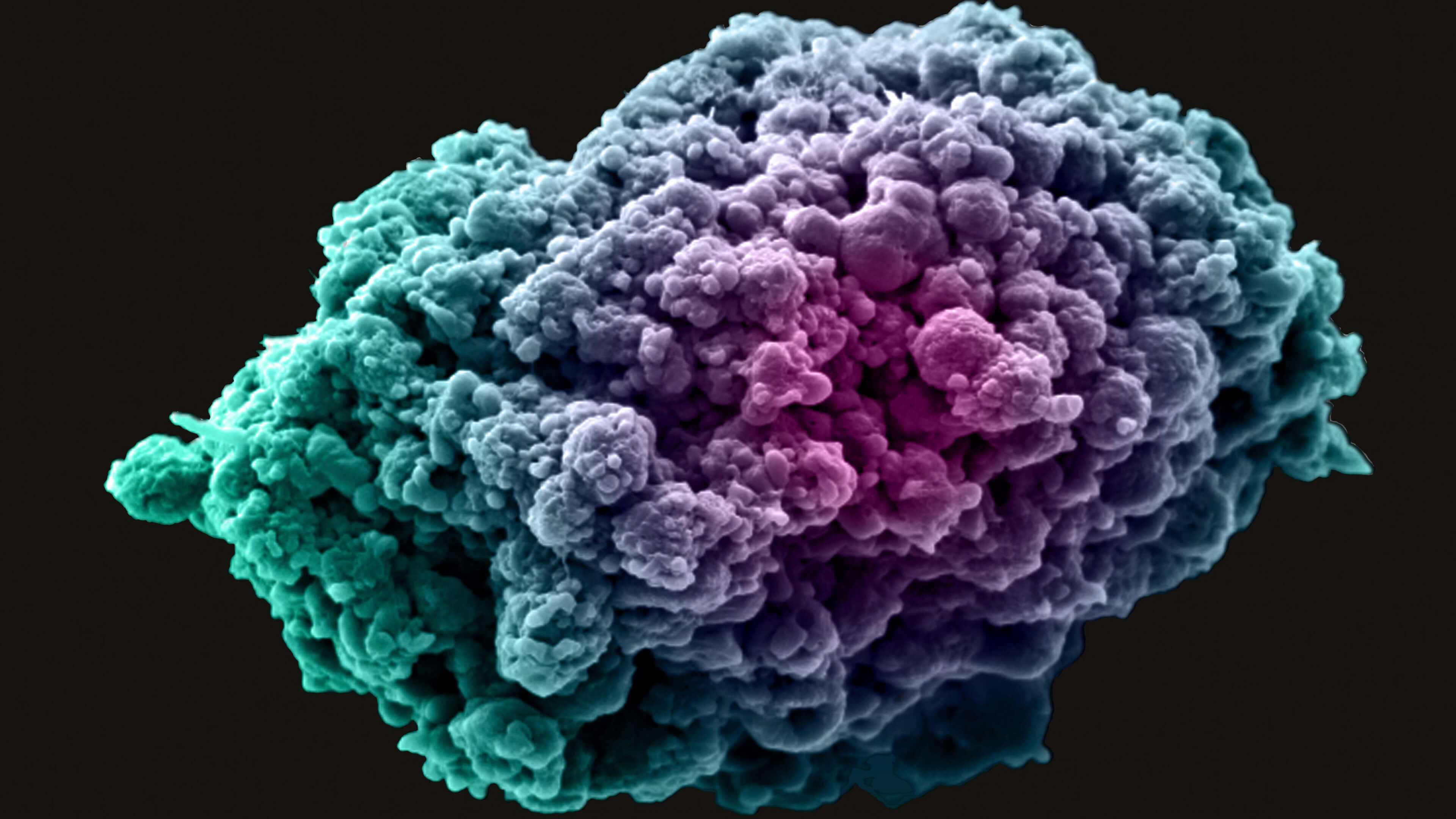
Capivasertib (trade name Truqap ▼) is a first-in-class drug that works by blocking the activity of the cancer driving protein molecule AKT.
Capivasertib was discovered by AstraZeneca subsequent to a collaboration with Astex Pharmaceuticals (and its collaboration with The Institute of Cancer Research (ICR) and Cancer Research Technology Limited).
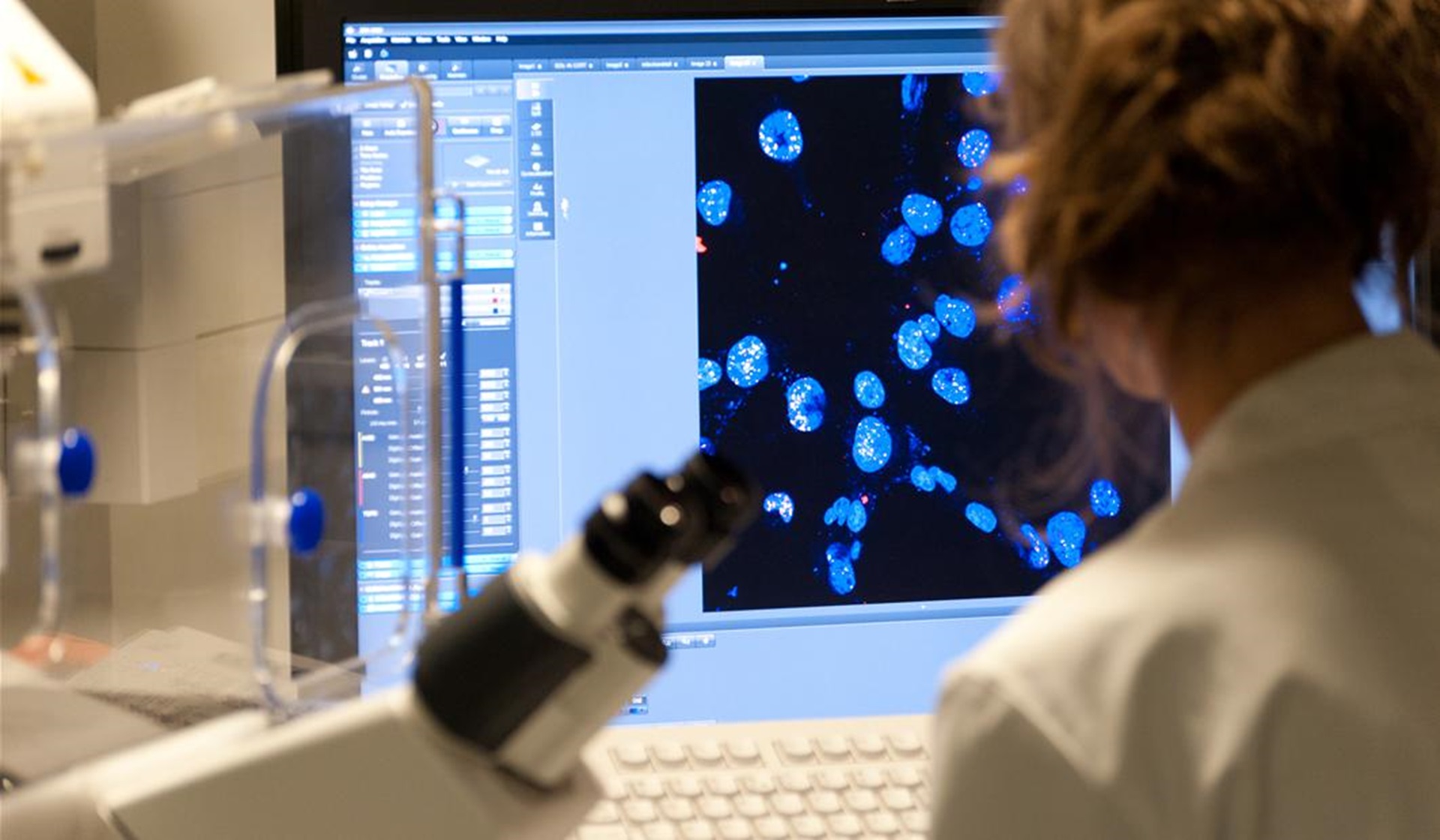
Working in the Breast Cancer Now Toby Robins Research Centre, Professor Nicholas Turner of the ICR and The Royal Marsden NHS Foundation Trust headed the international phase III CAPItello-291 trial, which led to its approval. The trial was sponsored and funded by AstraZeneca.
Results from the CAPItello-291 trial showed that capivasertib doubled the time it took for cancer to progress in people with advanced HR positive, HER-2 negative breast cancer with tumours PI3K, AKT, or PTEN alterations – from 3.1 months for patients who received hormone therapy alone, to 7.3 months for those who received hormone therapy combined with capivasertib.
Participants on the trial had experienced their cancer recur or progress despite standard hormone treatments, and the majority had also previously been treated with a CDK4/6 inhibitor – a class of drugs that stop cancer cells from multiplying.
In the UK, patients with advanced HR-positive HER-2 negative breast cancer are otherwise offered the option to continue to receive fulvestrant hormone therapy, which is often ineffective when given on its own, or chemotherapy, a treatment which carries debilitating side effects. There is great need for new treatment options.
Targeting the AKT protein
The development of capivasertib followed years of fundamental research at the ICR, aimed at understanding how the AKT protein is regulated. The AKT protein had been identified as an attractive target for anti-cancer drugs, due to its involvement in the growth and survival of cancer cells. In 2002, ICR scientists cracked and published the 3D structure of AKT and showed how the protein is activated.
Researchers in the ICR’s Centre for Cancer Drug Discovery, with funding from Cancer Research UK, then worked in collaboration with Astex Pharmaceuticals to design small-molecule inhibitors which would target AKT, based on its 3D structure.
In 2005, a series of prototype drug compounds discovered by the ICR and Astex was shown to have very promising activity against a range of human tumours grown in mice and was licensed to AstraZeneca. Then, in 2010, AstraZeneca announced its discovery of capivasertib and began to develop the drug as a potential treatment for various forms of cancer.
The initial clinical development of capivasertib was centred on an early-phase trial which was led by the ICR and its partner hospital The Royal Marsden. Subsequently, phase II studies were completed in the UK in collaboration with the UK Cancer Research Network.
The trials used biomarkers that were developed at the ICR to show proof of concept that the AKT protein was inhibited by capivasertib.
Patient case study – ‘My doctors say it is working and I feel that it is too – I feel so well.’

Elen, from Anglesey, worked as an NHS nurse and in social care for 30 years. She was diagnosed with primary invasive lobular breast cancer in 2008. After treatment which gave her eight years cancer-free, the disease has since returned in her bones, stomach and bowel. She has been taking capivasertib since February this year. She said:
“My nurses have described it to me as ‘groundbreaking’ and a ‘gamechanger’ – and for me it has been brilliant. I have had no side effects and it is much kinder than previous drugs I have been on. It is the only drug I have ever been able to take at the recommended dose without needing any adjustments. I am doing well on it. It has not affected my energy levels and my cancer markers are down, one of them by 50%. My doctors say it is working and I feel that it is too – I feel so well. It has given me hope. I would like to get at least two good years out of it.”
‘One of the most effective drugs we have seen’
Professor Nicholas Turner, Professor of Molecular Oncology at The Institute of Cancer Research, London, and Consultant Medical Oncologist at The Royal Marsden NHS Foundation Trust, who led the CAPItello-291 trial, said:
“This positive NICE recommendation means that thousands of NHS patients with advanced breast cancer with these specific biomarkers can now receive this innovative targeted treatment to keep their cancer from progressing for longer. It’s an immensely rewarding moment to see this drug provide patients with a treatment option and precious extra time with their families.
“It is now crucial that advanced breast cancer patients have their cancer tested to identify those who could benefit from this capivasertib combination.”
‘A triumph’
Professor Kristian Helin, Chief Executive of The Institute of Cancer Research, London, said:
"This announcement is a triumph that will improve treatment for these patients with the most common type of advanced breast cancer. Around half of patients with this kind of breast cancer have mutations in one or more of the genes and for these patients, capivasertib can halt disease progression. I’m delighted that access to the drug is being expanded to NHS patients in England and Wales who are in desperate need of better options.
“The approval is also a significant achievement for the ICR, and a great success story for British science. Decades of discovery science work and a major drug discovery project by ICR researchers, along with a crucial partnership with Astex Pharmaceuticals, paved the way to the discovery of capivasertib by AstraZeneca.”
‘Immensely gratifying’
Professor Paul Workman, former Chief Executive of The Institute of Cancer Research, London, and former Director of the Centre for Cancer Drug Discovery, and an active researcher in the AKT drug discovery project, said:
“I am delighted to celebrate this landmark moment and see capivasertib become available on the NHS. The drug’s discovery and development, following early fundamental research, has been a long scientific journey for myself, and the outstanding teams of scientists at the ICR, Astex and AstraZeneca. It’s immensely gratifying that years of collaboration have contributed to this new cancer drug, which has the potential to improve the lives of so many NHS patients living with advanced breast cancer."