Ovarian cancer continues to claim thousands of lives in the UK each year, despite being relatively treatable if it’s caught early. However, an innovative laboratory test – the liquid biopsy – could identify cancer cells before a tumour forms, transforming diagnosis and treatment and bringing new hope for patients. Isy Godfrey spoke with Dr Isaac Garcia-Murillas, who is leading research into this new diagnostic technique, to find out more.
People sometimes describe ovarian cancer as a ‘silent killer’, but this is arguably a misnomer. Although ovarian cancer is difficult to detect, that’s because it’s sneaky, not quiet. The disease does produce symptoms – persistent bloating, loss of appetite, abdominal pain and urinary urgency being among the most common – but these often point towards other conditions, such as irritable bowel syndrome and urinary tract infections.
Women who notice a lump in their breast will typically seek medical advice to rule out or confirm breast cancer. Similarly, unusual vaginal bleeding is known as a possible warning sign of cervical cancer. But, even though ovarian cancer is the sixth most common cancer in women in the UK, women are more likely to ignore or postpone a diagnosis for symptoms that they associate with less serious conditions.
This issue is perpetuated by the underlying ‘health gap’ that means women’s pain is typically taken less seriously than men’s, leading many women to feel as though their symptoms are dismissed by healthcare professionals. This can reduce the motivation to seek health advice.
As a result, in some areas of the UK, only 21.8 per cent of women with ovarian cancer receive their diagnosis when the disease is still at an early stage (stage I or II), despite studies showing that 90 per cent of women will have at least one symptom at this point. In England, 95 per cent of women diagnosed with stage I ovarian cancer will survive for five years or more, as will more than 70 per cent diagnosed at stage II. The survival rate decreases to about 30 per cent at stage III and only 15 per cent at stage IV.
With UK statistics showing that one woman is diagnosed with ovarian cancer every hour and that every two hours, a woman dies from the disease, we need to do better.
It only takes a moment to make a gift, but the impact of your donation can last a lifetime. Please donate today to help more women with cancer live longer, better lives.
So, could a noninvasive testing procedure known as a liquid biopsy be the answer? Dr Isaac Garcia-Murillas, Senior Staff Scientist in the Molecular Oncology Group at The Institute of Cancer Research, London, believes so.
He said: “In my mind, the next three to five years are going to be a game-changer. It’s exciting because that’s when we’re going to see these techniques moving from the experimental stage into the clinic, where they will benefit early-stage patients.”
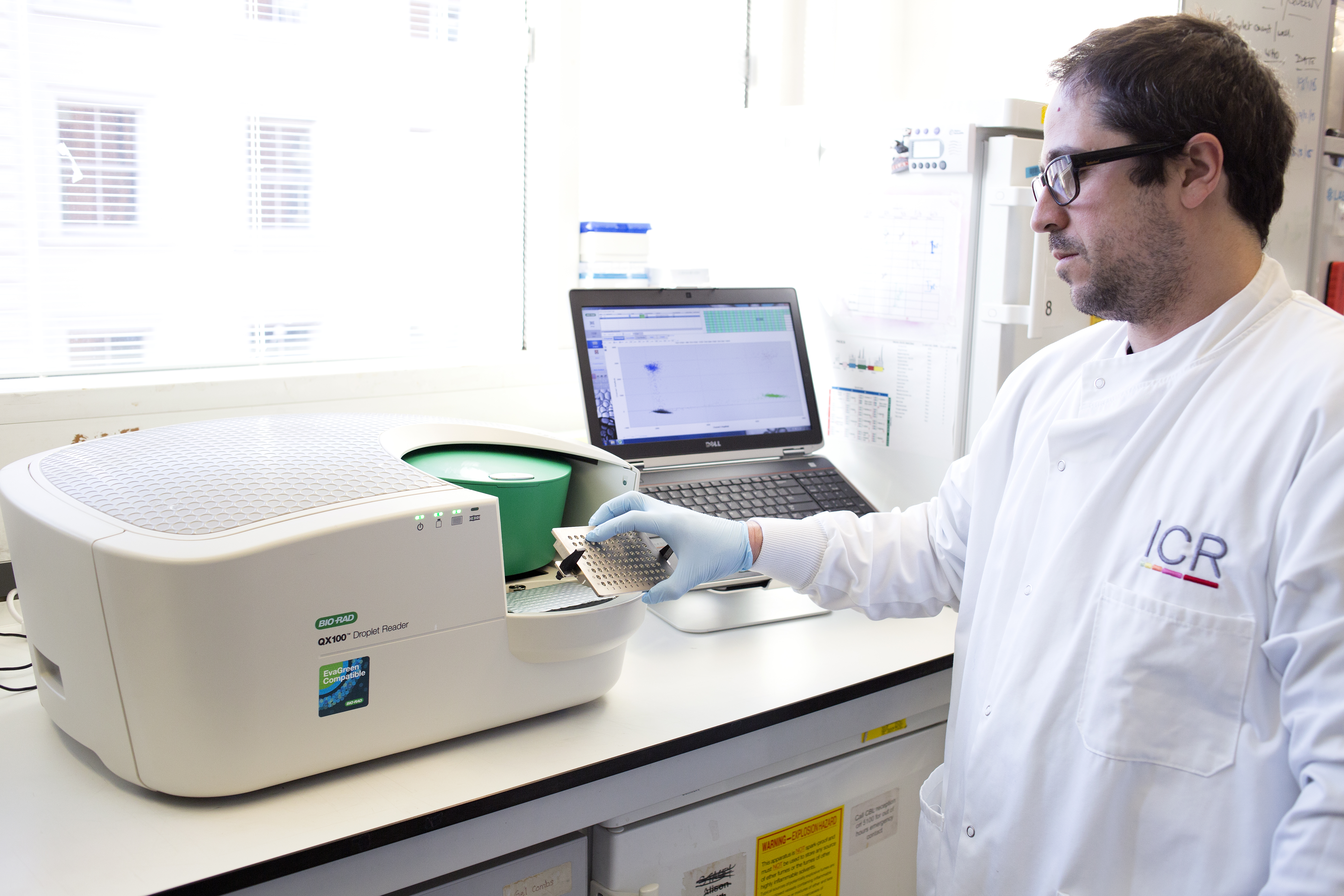
Image: Dr Isaac Garcia-Murillas working in the lab
What is a liquid biopsy?
Many people will have heard of a biopsy, in which a piece of tumour is removed for evaluation under a microscope. A liquid biopsy is similar, but it uses fluids from the body, so it is much less invasive.
The tests can work using any bodily fluid that might contain cell-free DNA, which is released into the bloodstream by cells as they die. Dying tumour cells will also release DNA – known as circulating tumour DNA (ctDNA) – into the bloodstream, so if ctDNA is detected in a liquid biopsy, scientists can use it both to confirm cancer and to discover genetic information about the disease.
Blood is the most commonly used bodily fluid, but liquid biopsies can sometimes be carried out using urine, cerebrospinal fluid and even saliva. Researchers have also explored other bodily fluids, using tears to look for uvea melanomas and breast milk to detect breast cancer in pregnant and postpartum women.
Find out about the ICR’s recent work on a blood test that predicts the recurrence of breast cancer ahead of relapse and a saliva test that can diagnose prostate cancer at an earlier stage.
Benefits for patients and providers alike
Liquid biopsies offer lots of benefits compared with standard biopsies. Dr Garcia-Murillas explained:
“The fact that these tests are non-invasive is of paramount importance, especially to patients. A tissue biopsy of the breast can be uncomfortable or even painful, while more difficult-to-obtain biopsies, such as those for prostate or lung cancer, have associated risks. Liquid biopsies are also faster and cheaper to perform, which is good news for healthcare providers.”
Liquid biopsies can also provide more information than tissue biopsies. Tissue biopsies generally only allow pathologists to analyse a small section of the suspected tumour, so they only have access to the genomics of that specific region. However, cells within a tumour are not all the same – instead they differ in terms of gene expression, size, structure and potential to spread, among other characteristics. Liquid biopsies are better able to capture this, giving scientists a much more comprehensive understanding of the tumour.
“The idea with liquid biopsies is that as cells die, they release the tumour DNA into local bodily fluids,” said Dr Garcia-Murillas. “You are capturing cell death in all regions of the tumour, so the mutational profile, for example, is more representative of the whole tumour.
“What’s more, in advanced disease, when you have multiple metastatic sites, if you just get a tissue biopsy of one of them, you’re not getting the full picture of the cancer. Cells at all of these sites will be releasing their contents when they die, so a liquid biopsy will better capture the genetic diversity within the different tumours.”
A tool with many possible uses
Liquid biopsies could have many uses in the clinical setting – both for ovarian cancer and for other solid tumours. In fact, these tests could have a role at multiple points in the patient journey.
Diagnosis and treatment
Initially, they can be used to confirm a diagnosis of cancer, which they can do at an early stage of the disease because cancerous cells start releasing ctDNA into bodily fluids before a solid mass forms.
Then, the unique genetic landscape of the tumour can guide treatment decisions, allowing patients, where possible, to receive appropriately targeted therapies. A better understanding of the cancer’s genetics can also help with predicting patient outlooks.
An interesting potential use for liquid biopsies further down the line is to monitor how a patient is responding to treatment, which is not feasible using tissue biopsies.
Dr Garcia-Murillas said:
“Tumours evolve, and we can’t monitor them continuously in real time. However, with a liquid biopsy, you can take blood every three or six months, or every cycle of therapy, which will allow you to look at tumour evolution over time. In comparison, with a tissue biopsy, a patient will have one for the primary tumour and one when the tumour is removed surgically, but they won’t have another until they’ve relapsed and have metastatic disease – if it’s accessible. You lose all the evolution information because there’s no way to monitor it in real time.”
This monitoring would also give clinicians more warning of a treatment regimen becoming ineffective, at which point they could change the approach. Currently, patients are not monitored until there is disease progression, showing that they are no longer responding to the treatment.
Following treatment
Liquid biopsies could also be beneficial once a person has completed treatment, by providing early warning of a relapse. A study led by Dr Garcia-Murillas – which was published in the journal Breast Cancer Research and Treatment – has already shown that ctDNA can successfully be used to predict breast cancer recurrence. The procedure can reveal whether a small number of cancer cells has remained in the body after seemingly curative treatment. These cells are so few in number that they cannot be detected by clinical examination or imaging. However, a liquid biopsy is sensitive enough to detect one cancer cell among a million noncancerous cells.
More recent work by Dr Garcia-Murillas, which was presented at the 2024 ASCO Annual Meeting, found that a newly developed type of liquid biopsy accurately predicted breast cancer relapse up to 41 months before clinical relapse, with the median lead time being 15 months.
“You have more than a year of a window of opportunity there to intervene,” said Dr Garcia-Murillas. “We are starting to see this molecular relapse way before you can detect any relapse by imaging, which is the standard clinical way of detecting which women have this outcome. That opens the opportunity to take action while any tumours are small and homogenous.
“At this point, the disease is likely to respond better to treatment, giving you the opportunity to intervene and potentially affect the outcome.”
Importantly, lower risk patients could also benefit from liquid biopsies. The test would identify those who have responded to the initial treatment and have no residual disease, meaning they could be spared unnecessary treatment. Instead, they could be monitored at regular intervals to check for ctDNA as a sign of potential recurrence.
“The field was not really developed”
Dr Garcia-Murillas joined the lab of Professor Nicholas Turner, Professor of Molecular Oncology at the ICR and Consultant Medical Oncologist at The Royal Marsden NHS Foundation Trust, more than a decade ago. Together, the scientists started to explore the possibility of capturing tumour genomics via a blood test. Their first project was to identify high expression levels of the HER2 gene in HER2-positive breast cancer, which then led to their ability to identify tumour mutations in ctDNA.
“The field was not really developed,” said Dr Garcia-Murillas. “We were one of the pioneer labs to show that you could use this technique to monitor and identify outcomes for patients. What attracted me most about this research was the potential to improve clinical care.”
Dr Garcia-Murillas works primarily on breast cancer, although his expertise has led to him providing a supporting role on projects in lung, prostate and colorectal cancer. He also has a particular interest in cancers of unmet need, so he collaborates with colleagues on thyroid cancer, head and neck cancer, and sarcomas.
He said:
“I really like the idea of being able to develop liquid biopsies not only for use in breast cancer but also in a wide variety of tumours, including ovarian cancer. When we started, just a handful of labs were involved, and now the whole thing has exploded because the likelihood of this approach improving health outcomes is so high. The broad uses of these tests will definitely benefit patients.
“You can do all the genomics and all this work without having to inconvenience patients by taking biopsies. Nobody likes having a biopsy taken. But a liquid biopsy is the same as going for a blood test.”
“It won’t be long until it’s changing patients’ lives”
Having been a pioneer in the field of liquid biopsies, Dr Garcia-Murillas is hoping to be in the rare position of taking a scientific technique from a concept right through to a clinical tool used as standard across multiple cancer types.
Across the field, the priority now is running prospective interventional clinical trials that are guided by liquid biopsies, potentially using a variety of bodily fluids. At the moment, these tests are only used for patients with metastatic breast cancer to identify the emergence of resistant mutations to a given therapy. But the ultimate aim is to use them across multiple cancers, including in the absence of a diagnosis and in the early stages of the disease. More data are needed to support clinical use here, as well as discussions around possible screening protocols.
However, Dr Garcia-Murillas is optimistic that it’s only a matter of time before we see liquid biopsies being used at all stages of cancer. He said:
“I’ve seen the evolution of the field, and there’s the ability now to develop all these new tests. It won’t be long until we can start changing patients’ lives, saying ‘you need treatment’, ‘you need more treatment’, ‘you need less treatment’, or ‘you need no treatment’.
A brighter future for people with ovarian cancer
Although much of the work on liquid biopsies has focused on breast cancer, researchers are increasingly interested in applying the findings to ovarian cancer.
The ICR’s Professor Turner has helped develop a highly sensitive blood test that detects changes in BRCA1 or BRCA2 genes in people with breast or ovarian cancer. These changes mean that the cancer will no longer respond to certain therapies, so clinicians can alter the treatment regimen before the cancer starts to progress.
Other research teams around the world are working on identifying a wider range of biomarkers that will allow the detection of ovarian cancer in the early stages. There is also interest in exploring the information that can be provided by other tumour elements, such as exosomes – tiny membrane-enclosed particles that serve as containers, transporting molecules between cells.
By contributing to the development of tools that can be used every day in the clinic to improve diagnosis and treatment, this research will translate into benefits for people living with ovarian cancer.
Once, a scenario in which we could diagnose ovarian cancer early and predict disease recurrence months ahead of clinical relapse would have seemed impossible. Now, thanks to liquid biopsies, it could be a reality within the next decade.
Using liquid biopsies effectively, we could save the lives of thousands of mothers, daughters, sisters, partners and friends.
You can help us get there by supporting our important work in liquid biopsies.