A bit like a balloon full of water, the bladder can expand and contract depending on how much urine is inside it – stretching to hold around 600-800 mL when full. Bladder shape, capacity and position vary between individuals, influenced in part by the neighbouring organs, making radiotherapy in patients with bladder cancer a real challenge. But now researchers at The Institute of Cancer Research, London, have been investigating how we can work with the bladder’s unpredictability to deliver better radiotherapy for a type of cancer that has traditionally been hard-to-treat.
Bladder cancer starts in the lining of the bladder, and is generally treated with surgery and chemotherapy. But when cancer cells spread beyond the inner lining of the bladder and into the muscle layer – becoming invasive bladder cancer – the most common treatment is a drastic procedure called a cystectomy. Dr Robert Huddart, leader of the Academic Radiotherapy and the Urology Unit at The Institute of Cancer Research (ICR) and Honorary Consultant in Urological Oncology at The Royal Marsden explains: “Radical cystectomy is where we remove the entire bladder, as well as nearby lymph nodes, part of the urethra, the prostate or the cervix and womb – something many people are understandably hesitant to undergo. Creating a new bladder from part of the intestine can be done, but this can often cause severe side-effects and patients usually end up wearing a plastic bag to collect urine.”
Thankfully, over recent years, treating invasive bladder cancer has been undergoing a renaissance, the start of which was initially driven by a trial led by the ICR. Researchers showed that combining chemotherapy and radiotherapy significantly improved patient outcome compared with radiotherapy alone. These results suggest that chemo-radiotherapy could be used as alternative to surgery.
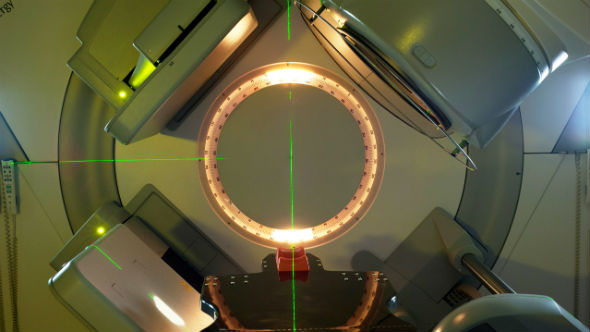
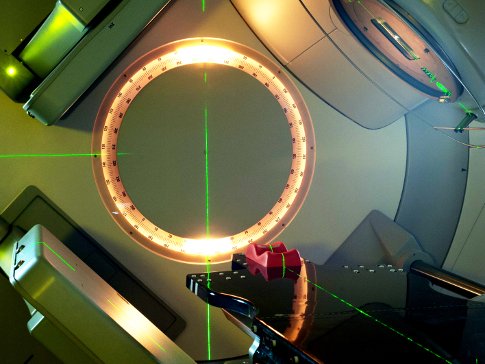
However radiotherapy to bladder can produce challenges. Before starting radiotherapy, doctors need to create a radiotherapy plan by scanning a patient’s bladder a few days ahead of treatment. By doing this, they can gather accurate information on the size and location of the tumour and radiation doses can be delivered effectively, causing as little damage as possible to the surrounding healthy tissue. But even with this detailed planning, there are still problems as Dr Huddart reveals. “We know that even when empty, the bladder will not be the same size, shape or in the same position for treatment as it was for the planning scan. Accounting for these changes, we use a large safety margin – typically 1.5 to 2.0cm – meaning we often irradiate larger areas than required. Despite this, parts of the tumour can still remain un-treated due to the changing size of the bladder coupled with the natural movement of organs in the body. And, radiotherapy-related toxicity occurs if we irradiate healthy organs, leading to side-effects such as the need to go to the toilet every hour and intense pain when urinating.”
Numerous studies are on-going that are seeking new ways for doctors to improve treatment planning. “In our APPLY study, we used simple CT scan pictures taken before each treatment to match the best treatment plan for the day from a library of radiotherapy plans,” Dr Huddart reveals. “Early results show that the new technique gave much better target coverage with improved normal tissue sparing. Because of the success of APPLY, we started the HYBRID trial that compares hypofractionated radiotherapy – radiotherapy given weekly using fewer fractions and higher doses rather than daily radiotherapy – with and without image-guided planning in patients with localised muscle invasive bladder cancer. Results should provide insights into if hypofractionated radiotherapy works in this patient population, and how well the treatment is tolerated. Patients selected for this trial were not considered fit enough to undergo daily radiotherapy or a cystectomy, so finding a treatment plan that works for this patient population will be really improving their outlook.”
Taking the research a step further, Dr Huddart and his team are using these new techniques to provide an extra radiotherapy ‘boost’ for patients receiving daily radiotherapy for bladder cancer. Dr Huddart says: “Using a CT scan before each treatment in our IDEAL study, we were able to increase the radiotherapy dose significantly, and deliver it precisely and safely. Based on our results, we received additional funding from Cancer Research UK – as part of their #nomakeup campaign – to support a trial called RAIDER, which will test our ideas across the UK, Australia and New Zealand. We hope this will start later this year.”
Historically, delivering effective radiotherapy has been a real challenge in bladder cancer. But now this looks set to change, as accurate, safe and effective treatment techniques are being tested that could make a huge difference to patients.
The APPLY and IDEAL trials are funded by our National Institute for Health Research Biomedical Research Centre for Cancer; HYBRID and RAIDER trials are funded by Cancer Research UK.