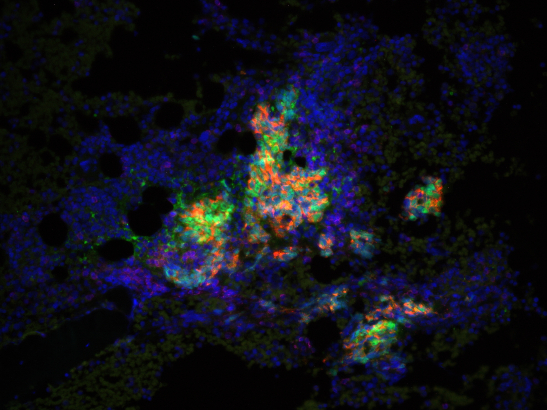
Image: Prostate cancer cells. Credit: Professor Johann de Bono, The Institute of Cancer Research, London.
Scientists have worked out a way of predicting how long a prostate cancer patient will continue to respond to the PARP inhibitor drug, olaparib, according to new research published in the journal Cancer Cell.
A team from The Institute of Cancer Research, London, used a simple blood test to detect the presence of genomic changes that affect how well the drug can act on cancer.
They saw a clear link between the number of certain DNA changes – called reversion mutations – a patient had and how long they survived.
The researchers also discovered that for patients with cancers missing the BRCA2 gene – who initially responded well to treatment – the cancer developed resistance to olaparib by regaining copies of this gene.
Results will pave the way to new treatments
PARP inhibitors such as olaparib have transformed treatment for advanced prostate cancer in recent years, but the length of time that patients respond to the medicine varies widely. The drug will eventually stop working for all patients and their cancers will continue to grow.
Being able to predict when – and how – patients will stop responding to a particular drug helps doctors to personalise treatment as it means they can switch patients to a different regimen. The researchers also hope the results will pave the way for the development of new drugs that target these genetic changes, preventing advanced prostate cancers from becoming resistant to treatment.
The researchers, funded by AstraZeneca, Prostate Cancer UK, Movember, Cancer Research UK and Prostate Cancer Foundation, analysed multiple blood samples from 25 patients with advanced prostate cancer who took part in the TOPARP-B clinical trial, who all initially responded well to olaparib. They looked for genomic changes in the tiny amounts of cancer DNA left in the body following treatment.
After just four months of olaparib treatment, scientists were able to see that patients with a high number of changes called reversion mutations had an average survival time of 13.9 months, compared to 21.4 months for those with a lower number of these changes.
PARP inhibitors such as olaparib work by stopping the cancer cell from repairing its DNA. The Phase II TOPARP-B trial, led by a team at The Institute of Cancer Research (ICR), and The Royal Marsden NHS Foundation Trust, and managed by the ICR’s Clinical Trials and Statistics Unit, tested the drug in metastatic castration-resistant prostate cancers which have mutations in or deletions of genes responsible for repairing DNA damage.
The clinical trial found that the people with mutations in BRCA1, BRCA2 and PALB2 genes responded well to olaparib. All patients did eventually see their cancer develop resistance to the drug, with the cancer growing again.
Understanding the mechanism of resistance
Studies in the lab have shown that cancers may develop resistance to olaparib through reversion mutations – which restore function back to the already mutated genes, enabling them to repair DNA. This is the first research to study the link between these mutations and clinical outcomes for prostate cancer patients.
Some patients who initially responded well to olaparib had tumours where the BRCA2 gene was completely missing. The researchers were surprised to discover that, after olaparib treatment, these patients’ tumours regained the missing gene and quickly developed resistance to the drug.
This research is the first to show how olaparib treatment drives some prostate cancers to restore the ability to repair DNA – even in tumours with missing BRCA2 genes, where there are no mutations to simply ‘reverse’.
Since these tumours have restored the ability to repair DNA, they wouldn’t be suitable for chemotherapy – a treatment which aims to damage DNA.
The researchers hope these findings will be used to develop treatments that prevent resistance to olaparib occurring, and to spare patients from treatments with harsh side effects that won’t work.
Personalise treatments to patients
Professor Johann de Bono, Regius Professor of Cancer Research at The Institute of Cancer Research, London, and Consultant Medical Oncologist at The Royal Marsden NHS Foundation Trust said:
“PARP inhibitors have transformed advanced prostate cancer care, but we need to stay one step ahead to prevent resistance developing. This research highlights that the tactics cancer uses to dodge the effect of olaparib can be spotted via a simple blood test. In time, I expect to see the development of drugs targeting these tumour adaptations, so that we can personalise treatment to patients and give them longer and better-quality lives.”
Professor Kristian Helin, Chief Executive of The Institute of Cancer Research, London, said:
“Drug resistance is one of the biggest problems we face in treating cancer. Knowing which cancers will develop resistance in advance means that we can move patients onto alternative treatments, or new combinations of treatments, to keep their cancer at bay for longer. This study gives us an insight into how this resistance to PARP inhibitors – such as olaparib – develops, and I look forward to seeing future research into targeting this mechanism.”
'Providing men with advanced prostate cancer more valuable time with their loved ones'
Simon Grieveson, Assistant Director of Research at Prostate Cancer UK, said:
“Being diagnosed with advanced prostate cancer can flip a man’s world upside down. In recent years we have seen the emergence of personalised treatments for men with advanced disease, where therapies are being selected based on the particular genetic characteristics of that man’s cancer. PARP inhibitors, such as olaparib, have demonstrated fantastic results for some men, however not all men respond to this drug and for those that do, their cancer eventually develops resistance.
“Prostate Cancer UK are thrilled to have funded this research in partnership with Movember as it reveals how treatment resistance to olaparib may develop. Through detecting particular markers in the blood, it may be possible to identify early those patients whose cancer is no longer responding to olaparib, so that alternative treatments can then be considered sooner. Further research is needed, however what’s also exciting is that this research suggests strategies which could potentially further delay, or even prevent, this kind of treatment resistance from occurring, providing men with advanced prostate cancer more valuable time with their loved ones.”