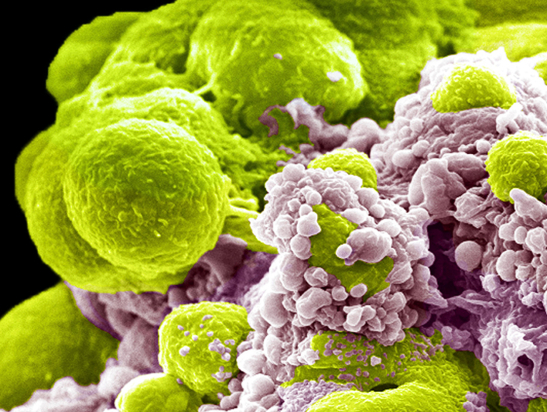
Image: Prostate cancer cells treated with nano-sized drug carriers. Credit: Wellcome Collection
Combining the principles of evolution with artificial intelligence (AI), scientists have proposed a new way to predict the chance of prostate cancer returning. In a recent study, they harnessed computational methods to capture specific tumour measurements relating to the tumour’s ability to change over time. They then showed that these measurements correlate with disease recurrence more than a decade after the initial diagnosis.
This approach could help clinicians systematically categorise patients according to their risk of disease recurrence. Based on this, they may be able to determine which patients only need localised treatment – typically radiotherapy, often alongside hormone therapy, or surgery – and which should receive additional treatment.
The study, led by researchers at The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust, could ultimately help clinicians better personalise treatment for prostate cancer. The findings, which have been published in Nature Cancer, were largely funded by Cancer Research UK, with additional funding from the Medical Research Council and the Wellcome Trust.
This work also uniquely combined certain tumour measurements in an evolutionary way, further validating the application of an evolutionary biology model to cancer. Scientists at the Centre for Evolution and Cancer at The Institute of Cancer Research (ICR) are at the forefront of cancer evolution research, which they are confident will lead to new effective treatments for multiple types of cancer.
Addressing the lack of predictive markers in prostate cancer
It is particularly difficult to predict outcomes in prostate cancer because the disease has extensive heterogeneity, meaning that there are significant differences between the cancerous cells – both within each tumour and across patients. In addition, cancer often develops at more than one site within the prostate, producing two or more tumours in proximity. As a result, it is often difficult for clinicians to determine the best treatments for their patients.
In some cases, clinicians can adopt a ‘watch-and-wait’ approach, sparing a person from the side effects of treatment while it is not necessary. However, this strategy could prove fatal for people with aggressive cancer or cancer that is more likely to recur.
Although other studies have evaluated the use of tumour measurements to predict outcomes, these used limited numbers of patient samples, only considered early-stage disease and were often not carried out in a clinical trial setting. In addition, they primarily included patients who had already undergone surgery to remove the cancer.
Believing that treatment decisions should be made ahead of surgery instead, the team behind the new study set out to find a new way to predict tumour progression in people diagnosed with high-risk locally advanced prostate cancer.
Identifying new measurements
The researchers used a form of AI called machine learning to analyse a total of 1,923 samples from 250 participants on the IMRT (intensity modulated radiotherapy) clinical trial, with a focus on the spatial tissue structure. They also used a purpose-built AI technique to perform Gleason grading – a scoring system that grades cancerous tissue from one to five based on the pattern of its cells. Cancerous cells that look very similar to healthy cells are assigned grade one while those that look significantly different are assigned grade five.
At the same time, the researchers assessed the genetic differences between the cells within individual tumours, using 642 samples from 114 participants in radiotherapy trials at The Royal Marsden. These samples overlapped with the first set, providing the team with integrated information about the cells’ genomics and morphology, as well as the patients’ outcomes over more than a decade.
The researchers found genetic divergence and AI-measured morphological diversity (the difference in the shape, size and structure of the cells) to be indicative of the tumour’s ability to evolve, which allows the disease to adapt and survive. They measured this diversity by looking at the extent of the differences between cells in different areas of the tumour, known as intra-tumour heterogeneity.
The findings showed that this ‘evolvability’ was a strong predictor of recurrence, with the combination of the two measurements identifying a subgroup of patients who experienced disease recurrence in half the length of time compared with the rest of the patients.
The team was also able to identify a correlation between the loss of a specific chromosome and a reduced presence of immune cells in the tumour, which may affect its response to certain treatments. This additional information could further support better treatment decisions.
The next step is for the researchers to test their evolution-based measurements of recurrence risk in a larger group of people with a broader range of disease characteristics. They will also need to factor in external factors, such as hormone levels.
“New methods such as ours are urgently needed”
Joint first author Dr George Cresswell, who was a Postdoctoral Research Fellow in the Genomics and Evolutionary Dynamics group at the ICR when the research was carried out and is now Principal Investigator at St. Anna Children’s Cancer Research Institute in Vienna, Austria, said:
“We are pleased to have found new measurements that can be taken from standard prostate cancer biopsies to predict the risk of recurrence in people with prostate cancer. Doctors don’t currently have specific enough ways to measure which patients have the lowest and highest risk of their cancer returning, meaning new methods such as ours are urgently needed.
“Our work has also demonstrated the combined potential of evolutionary genomics and artificial intelligence to enhance our study of cancer tissues when we apply it in the context of clinical trials. We hope that this approach will accelerate our progress towards using evolutionary biomarkers in clinical practice for both prostate cancer and other types of cancer.”
Joint senior author Professor David Dearnaley, Emeritus Professor at the ICR and retired Consultant Clinical Oncologist at The Royal Marsden, said:
“This study shows the power of a combined approach in which we assess both genomics and spatial morphology. We believe that our findings will make it possible to identify the patients with high-risk localised cancer who are most likely to benefit from early treatment with life-extending medications. Until now, we’ve not been able to separate out the patients who have the very highest risk of recurrence, but our novel analyses could change this by significantly improving our ability to predict whether cancer will return.”
The other senior author, Professor Andrea Sottoriva, Professor of Cancer Genomics and Evolution at the ICR at the time of the research and now Head of the Computational Biology Research Centre at Human Technopole in Milan, Italy, said:
“It’s exciting that we have taken new measurements with innovative evolutionary interpretations that have never been shown before. As well as producing better prognostic biomarkers for prostate cancer, our study serves as additional evidence that the evolutionary biology paradigm applied to cancer has a remarkable predictive power.
"By applying a computational approach to multiple datasets, we have been able to decipher some of the dynamics of cancer progression and treatment resistance. This type of research is key to furthering our understanding of how and when to treat cancers, including prostate cancer."