A new study is uncovering the evolutionary history of multiple myeloma for the first time, according to researchers.
Scientists at The Institute of Cancer Research, London, screened patients with a common type of multiple myeloma, and found that between two and six genetic mutations were driving the formation of their tumours, which grow into distinct populations of cancer cells in the body.
They also saw that within the same environment, independent groups of cancer cells may evolve in parallel to acquire similar mutations.
The findings reveal a snapshot of how myeloma evolves from a set of genetic abnormalities, which could have profound implications for how we treat this common type of blood cancer.
The study, published in the Journal Leukemia, was funded by Cancer Research UK, with additional funding from the NIHR Biomedical Research Centre at The Royal Marsden Hospital and Myeloma UK.
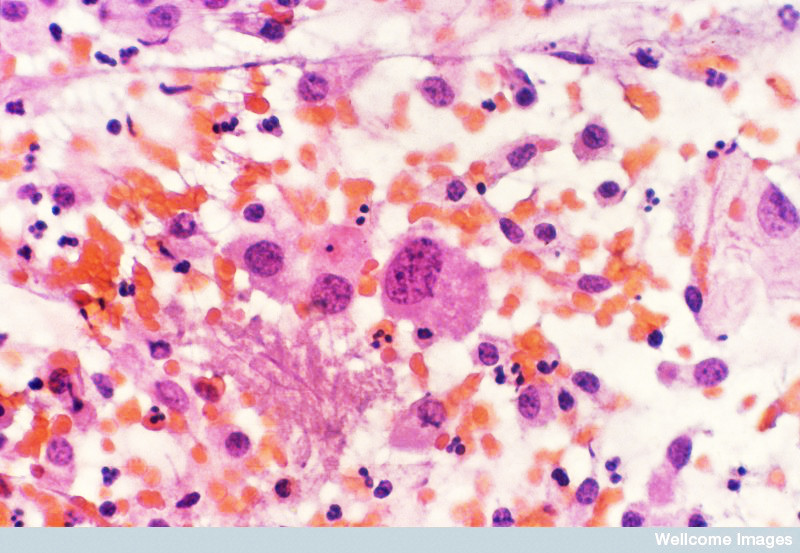
The transformation of a normal cell into a cancer cell occurs through a series of genetic changes to its DNA. The tumour environment puts selective pressures on cells, causing them to diversify as they evolve over time.
The same process is known to happen in myeloma, a blood cancer that is diagnosed in nearly 4,700 people in the UK each year, but until now there had been no direct evidence showing this evolution.
Scientists from The Institute of Cancer Research (ICR) used whole exome sequencing, which looks at the regions of DNA that make proteins, and single cell genetic analysis, to create the first maps of how myeloma evolves.
They studied six patients with t(11;14) translocations, a common cause of myeloma where two chromosome fragments fuse together abnormally, and recorded the incidence of several well documented mutations in individual cells.
The researchers found that before treatment, each patient had between two and six distinct cell populations, or clones, within their tumours. Each clone had a unique set of mutations, which are expected to cause them to respond differently to treatment.
Comparing whole exome sequencing data against their single cell analysis, they saw that some patients’ tumours possessed clones where each mutation was acquired linearly, while other patients’ clones had evolved in a branching pattern.
They also saw for the first time evidence of parallel evolution in three myeloma patients, where two clones mutated independently to possess defects in the RAS/MAPK pathway at the same time. Errors on this pathway can lead to uncontrolled cell growth, which is a hallmark of cancer.
The researchers then compared samples from a patient with plasma cell leukaemia, the most serious form of myeloma, before treatment and after their condition had relapsed. They saw that initially the patient had 4 major clones, but while treatment killed some, other clones were able to survive and flourish in their absence. These clones originated from the earliest ancestral clone, which wasn’t detectable at diagnosis, suggesting that earlier ancestral clones may be responsible when patients relapse.
The findings could be used to identify the key mutations that occur early in the development of myeloma, allowing doctors to use targeted treatments more effectively.
First author, Dr Lorenzo Melchor, Post-Doctoral Training Fellow in Molecular Haematology at the ICR said: “This is the first time that multiple myeloma evolution has been investigated at the single cell level, giving us a snapshot of how the disease grows from a handful of mutations. This study also raises interesting questions for targeted cancer treatment.
“Targeted treatments aim to kill cancer by attacking specific mutations, but our study shows that this isn’t enough. Mutations from the earliest stages of the disease may persist throughout myeloma’s progression, and if you don’t target these mutations, your cancer will return.
“In the future, tracking myeloma’s evolution will help us target mutations shared among all sub-populations of cancer cells, or to positively select for mutations that are the most treatable.”