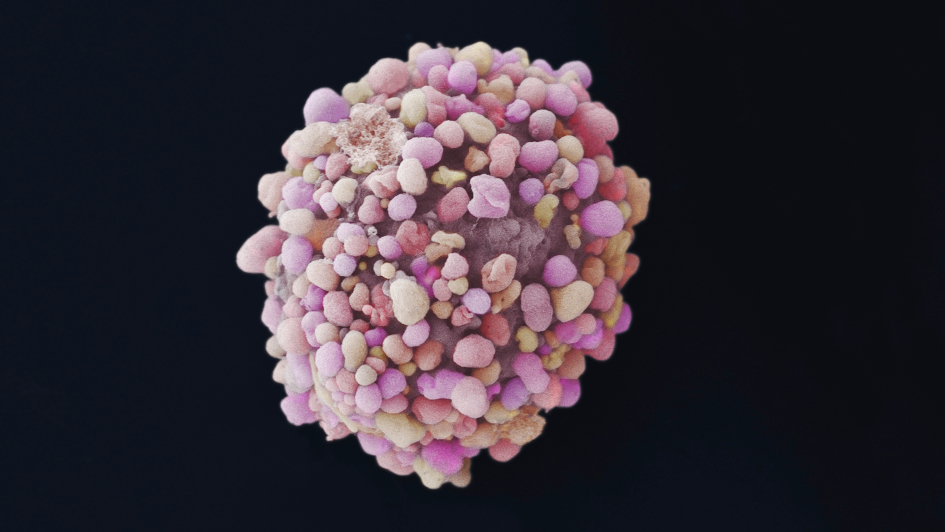
Image: Breast cancer cell. Image credit: Anne Weston, Francis Crick Institute via the Wellcome Collection. Licence: CC BY-NC.
A new type of drug that blocks one of cancer’s key evolutionary escape routes from chemotherapy could be used to treat aggressive breast cancers, a new study has shown.
Scientists at The Institute of Cancer Research, London, found that the drug could reinvigorate the response to chemotherapy in cancers that had become resistant, in both cells grown in the lab and in mice.
The drug is being developed in collaboration with the company Boston Pharmaceuticals following a licensing agreement and is currently in a phase I trial, after originally being discovered in the Cancer Research UK Therapeutics Unit at the ICR thanks to funding from partners including Cancer Research UK, the Cancer Research Technology (CRT) Pioneer Fund, Sixth Element Capital and Breast Cancer Now.
The drug, known as BOS172722, works by forcing cancer cells through cell division too quickly – leading to fatal errors in parcelling out DNA.
The first clinical trial of the new treatment is now under way in solid tumours including aggressive triple-negative breast cancers – and the researchers believe it might also be effective against other fast-growing cancers including ovarian cancer.
The new study is published in the journal Molecular Cancer Therapeutics and was funded by The Institute of Cancer Research (ICR) – a charity and research institute – as well as by Cancer Research UK, Breast Cancer Now and Sixth Element Capital LLP.
BOS172722 is an example of one of the new evolution-busting therapies that will be the focus of the ICR’s planned £75 million Centre for Cancer Drug Discovery.
The centre is a £75m project – and we now have less than £14m to raise. To make our building a reality, we urgently need your philanthropic support.
Drug blocks key player in cell division
The drug was discovered at the ICR in the Cancer Research UK Cancer Therapeutics Unit. It blocks a molecule called MPS1, which plays a central role in controlling cell division.
MPS1 is involved in organisation of chromosomes during cell division, ensuring they are distributed correctly between daughter cells and making sure that cell division doesn’t go ahead until they have been parcelled out evenly.
By blocking MPS1 using the new drugs, cancer cells speed through cell division with the wrong number of chromosomes and die as a consequence.
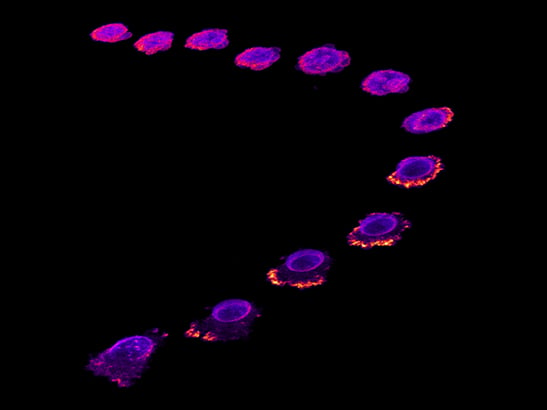
The ICR researchers found that cancer cells in dishes treated with the MPS1 inhibitor went through cell division in just 11 minutes, compared with 52 minutes without the drug.
And fast-dividing cells, from triple-negative breast cancers, ovarian and lung cancers, were especially sensitive to the effects of blocking MPS1.
Currently, people with triple-negative breast cancer receive taxane chemotherapies, such as paclitaxel, as their standard care. Paclitaxel also affects the distribution of chromosomes during cell division but blocks the cell from dividing, which causes the cell to die. However, some cells escape becoming resistant to the drug and giving rise to more tumours.
Phase I trial under way
Treatment with paclitaxel in combination with BOS172722 dramatically reduced time in cell division – from 110 minutes with paclitaxel alone to 15 minutes when combined with BOS172722. All cells treated with the combination divided with gross chromosomal abnormalities and died as a result, whereas 40 per cent remained alive with paclitaxel alone.
The MPS1 inhibitor was also effective at lower doses when used in combination with paclitaxel in mice, and was well tolerated by mice at the doses that almost completely eliminated the tumours.
Professor Spiros Linardopoulos, Professor of Cancer Biology and Therapeutics at The Institute of Cancer Research, London, who led the study, said:
“We have discovered a brand new type of cancer treatment that uses cancer’s rapid growth against it, by forcing cells through cell division so quickly that they accumulate fatal errors. The drug works especially well in combination with chemotherapy in triple negative breast cancer cells – the deadliest form of breast cancer for which there are few successful treatments.
“Crucially, the combination is anticipated to be effective in cancer patients that have already become resistant to chemotherapy alone and has the potential to become a much-needed extra treatment option that could extend the lives of patients.
“The phase I trial of this combination is currently well under way and I look forward to the results.”
World's first ‘Darwinian’ drug discovery programme
Professor Rajesh Chopra, Director of Cancer Therapeutics in the new Centre for Cancer Drug Discovery, said:
“Cancer’s ability to evolve and become drug resistant is the cause of the vast majority of deaths from the disease. We plan to counter that ability with the world’s first ‘Darwinian’ drug discovery programme within our Centre for Cancer Drug Discovery, dedicated to creating a new generation of anti-evolution treatments.
“Our new MPS1 inhibitor is a great example of a drug that seeks to outsmart cancer by blocking off a key evolutionary escape route, and in doing so we believe it can breathe new life into a chemotherapy that had ceased to be effective.”
Baroness Delyth Morgan, Chief Executive at Breast Cancer Now, which helped to fund the study, said:
“It's really promising that combining this newly-discovered drug with a standard chemotherapy could, in future, provide a new way to treat triple negative breast cancer and may even prevent the disease from becoming resistant to treatment.
“With triple negative breast cancer still lacking in targeted treatments, we urgently need to find new options to stop more women dying. This exciting study shows how well these drugs complement each other at a molecular level to destroy cancer cells.
“We now look forward to the results of clinical trials to understand whether this approach may be as effective and safe in humans. In the meantime, anyone with questions about their breast cancer treatment can call our free Helpline on 0808 800 6000 to speak to one of our expert nurses.”