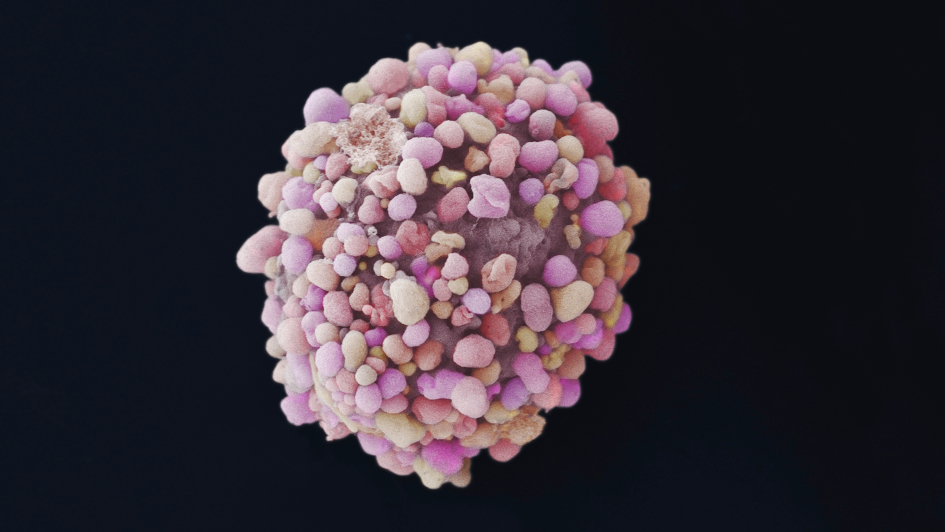
Image: Breast cancer cells. Credit: Annie Cavanagh. CC BY-NC 4.0
The Institute of Cancer Research, London, has hailed the ‘life-changing’ decision by NICE to recommend that the targeted drug olaparib can be used for NHS patients with both early-stage breast cancer and prostate cancer.
The keenly awaited judgement makes this pioneering treatment available for forms of breast and prostate cancer caused by faulty BRCA1 or BRCA2 genes – and offers the chance of longer, healthier lives for thousands of patients.
The recommendation will grant people in England and Wales with early-stage, high-risk breast cancer and inherited mutations in BRCA1 or BRCA2 access to olaparib following standard treatment – helping prevent their cancer returning and improving their chances of survival.
Men in England and Wales with advanced, incurable prostate cancer who have BRCA1/2 mutations in their tumours and who have seen their cancer progress despite hormone therapy will also have access to olaparib – delaying progression of their disease and keeping them alive for longer.
Flexible approaches to drug pricing
Experts at The Institute of Cancer Research (ICR) thanked NHS England and manufacturer AstraZeneca for reaching agreement following complex negotiations over how to price olaparib for different groups of cancer patients.
The ICR believes that more flexible approaches to pricing drugs for different indications will play a vital role in efforts to enhance access to new medicines on the NHS.
Olaparib is a precision medicine that belongs to a class of drugs called PARP inhibitors. It targets the specific biology of cancers linked to faulty BRCA1 or BRCA2 genes and works across many different cancer types.
Widening access to olaparib
Olaparib has been available on the NHS in England and Wales for women with advanced ovarian cancer, and inherited BRCA1 or BRCA2 mutations, who have stopped responding to treatment since January 2020. In Scotland, it has been available for these patients since July 2021 and has also been available for men with advanced, hormone-relapsed prostate cancer whose tumours have mutations in BRCA1 or BRCA2, since October 2021.
Olaparib is also licensed for use in patients with BRCA1 and BRCA2 mutations and advanced breast and pancreatic cancer, but it is not yet available on the NHS. Widening access to olaparib on the NHS to patients with BRCA1/2 mutation associated cancers across the UK has and continues to be a challenge, despite its development being a major success story for science in this country. Today’s news is a very significant forward step in translating olaparib’s benefits to NHS patients with early breast cancer and advanced prostate cancer.
The ICR has played a crucial role in the development of olaparib. ICR scientists were the first to demonstrate that cancer cells with mutations in BRCA1 or BRCA2 were highly susceptible to PARP inhibitors like olaparib.
Clinical trials of olaparib, led by researchers from the ICR and The Royal Marsden NHS Foundation Trust, then showed that olaparib was effective for patients with a range of cancers associated with BRCA1 or BRCA2 mutations.
'An amazing moment in a long scientific journey'
Professor Andrew Tutt was part of the ICR team at the Breast Cancer Now Toby Robins Research Centre that carried our early laboratory work which revealed how PARP inhibitors could target cancers with mutations in BRCA1 and BRCA2. He was also the lead Principal Investigator of the phase III OlympiA trial, coordinated globally by the Breast International Group, which revealed the benefits of olaparib in improving the chances of surviving high risk early-stage breast cancer.
Professor Andrew Tutt, Professor of Breast Oncology at The Institute of Cancer Research, London, and King’s College London, said:
“This is an amazing moment in a long scientific journey – starting with the discovery of the BRCA1 and BRCA2 genes more than 25 years ago, to ICR scientists identifying how to target a weakness in these cancers 10 years later, all the way through to the completion of the phase III clinical trials which led to today’s recommendations. It is immensely satisfying to know this work will now allow patients within the NHS to join the many thousands of patients globally whose lives are transformed by this work.”
Olaparib is a game-changing treatment for many people with cancers linked to inherited BRCA1 and BRCA2 genes.
Find out how olaparib is transforming patients' lives.
'These recommendations will be life-changing'
Professor Johann De Bono’s team were the first to administer olaparib to patients in clinical trials. Professor De Bono also led the Phase II TOPARP trials, and the phase III PROfound trial, which showed that giving olaparib to men with tumours that had weaknesses in DNA repair including BRCA1/2 mutations blocked prostate cancer growth, improved survival, and delayed disease progression.
Professor Johann De Bono, Professor in Experimental Cancer Medicine at The Institute of Cancer Research, London, and Consultant Medical Oncologist at The Royal Marsden NHS Foundation Trust, said:
“Olaparib is a precision medicine which extends the lives of men with advanced prostate cancer who have mutations in their BRCA genes. It is tremendously exciting to see the NHS in England and Wales make olaparib available to men suffering from these diseases. Olaparib is an important example of how understanding the underlying genetics of patients, and their tumours’ genomics, can be used to design highly targeted precision medicines.
“For patients with advanced prostate cancer and mutations in BRCA1 or BRCA2, these recommendations will be life changing – giving men another treatment option and precious extra time with their families, without the debilitating side effects we see with chemotherapy.”
'A momentous development in the treatment of cancers linked to faulty BRCA1 and BRCA2 genes'
Professor Kristian Helin, Chief Executive of The Institute of Cancer Research, London said:
“This is a momentous development in the treatment of cancers linked to faulty BRCA1 and BRCA2 genes. I am delighted that access to olaparib on the NHS, the first cancer drug in the world to target an inherited genetic fault, is being expanded to more patients who are in desperate need of better options. It’s great that NHS England and AstraZeneca have reached agreement on the pricing of olaparib, and it’s possible that this could prove a model for future access arrangements for drugs across multiple cancers.”
“Olaparib is a true example of how outstanding scientific research improves lives. More than 25 years of research at the ICR into understanding the underlying cause of these inherited cancers – involving partnerships between academia, industry and charities across the world to deliver clinical trials – has led us to a cutting-edge treatment which exploits the very mutation that caused the cancer.”
'Telling my children about my breast cancer was the hardest thing I ever had to do'
Annie Baker, 42, lives in Brockley, London, with her husband, Phil, 12-year-old daughter, Lizzie, and ten-year-old son, Patrick. She was diagnosed with early-stage breast cancer two years ago. She said:
“I was going through treatment and decided to go for genetic testing. I wasn’t automatically eligible for it, but I arranged it myself, and it was found that I had the BRCA2 mutation.
“In July 2020 I’d been diagnosed after finding a lump. After a biopsy I learned the cancer had spread to my lymph nodes. So I started chemo for five months and had a mastectomy in February 2021. There was still some cancer in the lymph nodes, so I went in for another surgery and after that no further cancer was found. Then I had radiotherapy and started on hormone treatment.
“Just after that I got my BRCA 2 results. I was aware of olaparib and the OlympiA clinical trial and was able to be part of AstraZeneca’s Early Access Programme.
“I started taking olaparib at the end of September 2021. I took it as tablets twice a day for twelve four-week cycles. And I felt a little queasy and tired sometimes, but my normal life continued. It was a sharp contrast to the chemo, which was really tricky and I lost my hair, or with the surgery which was life-changing.
.jpg)
Image: Annie with her children in the Lake District. Credit: Annie Baker
“I took olaparib for a year and during that treatment I worked full-time, completed a 10k, was a mum to my children and basically my normal self.
“And the amazing thing is that it’s reduced my risk of the cancer coming back. It’s incredible that I’ve been able to take this treatment while living and working as normal and it’s made such a huge change to my prognosis.
“Telling my children about my breast cancer was the hardest thing I ever had to do…and olaparib has really reduced the chances I will ever have to do that again.
“Olaparib has given me so much reassurance and hope. I feel so grateful to have been able to have this treatment.”
The development of olaparib was underpinned by more than 25 years of research at the ICR. We are working to develop targeted treatments for all types of cancer.
.jpg?sfvrsn=b8be1e0b_2)