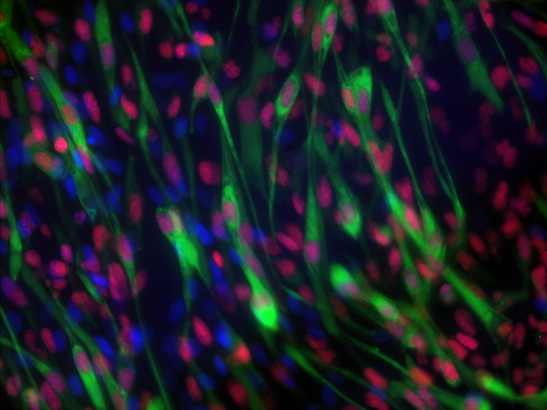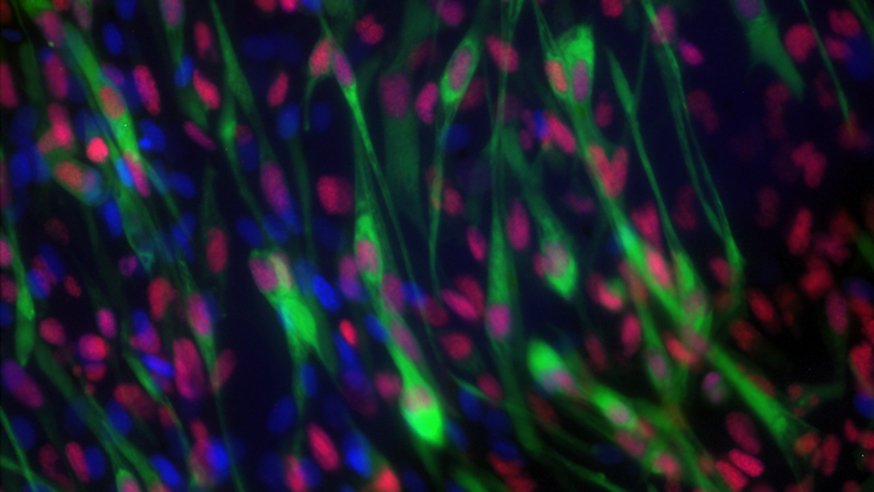
Image: Rhabdomyosarcoma cells. Credit: Dr Ewa Aladowicz, ICR.
A simple blood test could help guide the treatment of children with the cancer rhabdomyosarcoma, a new study reports.
Researchers found that ‘liquid biopsy’ blood tests could pick up signs that a cancer had returned, assess the severity of the disease, and help guide choice of drugs.
Around three-quarters of the children assessed with blood tests before treatment showed key genetic changes in their cancers – some of which could have implications for the children’s treatment.
International pilot study leads to larger trial
The promising findings are part of an international collaborative pilot study which is already being taken forward into a large international clinical trial.
Rhabdomyosarcoma is a rare type of cancer that mostly affects children. Less than a third of these children who relapse or whose cancer has spread will survive.
The study, led by scientists at The Institute of Cancer Research, London, involved blood and tissue samples from 28 patients with rhabdomyosarcoma from different centres across Europe, as well as studies in mice.
Measuring circulating tumour DNA
Researchers assessed whether measuring DNA shed by cancer cells into the bloodstream could track tumour progression and aggressiveness and be a faster and less painful alternative for children than traditional tissue biopsies.
The study, which received funding from Alice’s Arc, the KickCancer Foundation and the King Baudouin Foundation, is published in the Journal of Clinical Oncology – Precision Oncology.
Before analysing patient samples, researchers first assessed liquid biopsies in mice in the lab. They were able to successfully detect and monitor tumour growth by measuring circulating tumour DNA in mice with rhabdomyosarcoma. The study showed mice could be used to test treatment strategies using liquid biopsies before taking them to patients.
Three quarters of children showed key genetic changes
Researchers then looked at patient samples. Some 18 children in the study had blood samples collected prior to treatment and multiple blood tests taken during their treatment to track how their disease progressed.
Around three-quarters (14 out of 18) of children assessed with blood tests before treatment showed key genetic changes in their cancers. Some genetic changes could change their care, such as mutations in genes called MYOD1 and TP53 which are linked to rapid progression of rhabdomyosarcoma. These patients may benefit from more aggressive treatment.
Researchers also found that levels of cancer DNA circulating in the bloodstream before treatment were higher in patients whose cancer had spread to the lymph nodes and other parts of the body compared with patients whose cancers had not spread. The same was true for cancers found in a harder-to-treat regions of the body versus those in more favourable locations.
Predicting response to treatment
Researchers believe detecting increasing levels of circulating tumour DNA in the blood predicts poor responses to treatment. Using liquid biopsies to monitor patients could successfully determine how well treatment is working and identify patients who may need further interventions.
Various studies have shown that liquid biopsies can be used to monitor adult cancers like breast and prostate cancers – but research looking at their use in childhood cancers is more limited. This feasibility study shows the potential benefits of using liquid biopsies to track the childhood cancer rhabdomyosarcoma.
While the findings are promising, the pilot study involves a small number of patients and researchers caution that the findings should be validated in a larger clinical trial – which they are already planning to launch internationally next month.
The ICR is leading in the study of cancers in children, teenagers and young adults. Our researchers, supported by our family charity partners, play a key role in international research efforts that are transforming how these devastating diseases are treated.
'A key tool to judge prognosis and guide treatment'
Study leader Professor Janet Shipley, Professor of Molecular Pathology at The Institute of Cancer Research, London, said:
“Liquid biopsies have the potential to transform how we monitor and treat children with rhabdomyosarcoma. We hope that these simple blood tests can become a less invasive alternative to tissue biopsies, and a key tool to help judge prognosis and guide treatment.
“Our early pilot findings suggest that liquid biopsies can detect early signs of relapse, assess the severity of disease and help guide choice of drug treatment. We’re excited to be taking these findings into an international clinical trial involving larger numbers of children, and we hope we can realise the potential of using liquid biopsies to make children’s cancer treatment smarter and kinder.”
'Providing tailored treatment'
Professor Kristian Helin, Chief Executive of The Institute of Cancer Research, London, said:
“We are excited about the potential that liquid biopsies have to improve cancer treatment. It allows us to closely and sensitively monitor how the disease evolves over time. We hope these blood tests can help doctors to treat cancer patients, by predicting and rapidly responding to tumour development. It’s very encouraging to see liquid biopsy technology applied to children with rhabdomyosarcoma, and I hope it can help in providing tailored treatment for these patients, and ultimately increasing survival.”
'A complete game changer'
Alice Wakeling was seven years old when she died from rhabdomyosarcoma. Her parents Sara and David Wakeling set up the charity Alice's Arc to fund research to find a cure and develop kinder treatments for rhabdomyosarcoma. Sara and David said:
"This research is incredibly important to families impacted by rhabdomyosarcoma and the findings of the pilot study are promising. The possibility of being able to detect and predict the path of the disease via a blood test would be a complete game changer. It is about time that this became common practice for childhood cancers like rhabdomyosarcoma. It is a far more efficient and less invasive way to monitor disease in these children. We are delighted to continue investing funds into the next stage of the research to test these findings in the setting of an international clinical trial."