Some treatments for prostate cancer, while initially effective at controlling the disease, not only stop working over time but actually start driving tumour growth, a major new study shows.
Researchers identified the emergence of drug-resistant cancer cells by testing repeated blood samples from patients with advanced prostate cancer.
They set out a new ‘treatment paradigm’ – the constant monitoring of patients using a blood test for signs that therapy is becoming counter-productive.
The study was conducted at The Institute of Cancer Research, London, The Royal Marsden NHS Foundation Trust and the University of Trento in Italy.
It was mainly funded by Prostate Cancer UK with support from the Movember Foundation and Cancer Research UK, and is published today (Wednesday) in Science Translational Medicine.
The research showed use of glucocorticoids – steroid drugs often given alongside hormonal therapy – coincided with the emergence of mutations that resulted in the drug become an activator of the disease rather than an inhibitor.
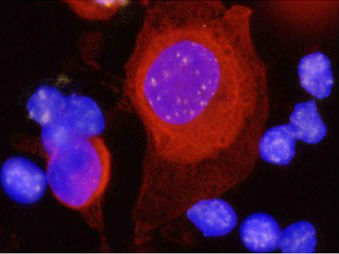
The results also provide robust evidence that ‘liquid biopsies’ analysing tumour DNA circulating in blood could give an accurate picture of cancer development in individual patients.
The findings suggest that in future, men with advanced prostate cancer could be carefully monitored for circulating tumour DNA, allowing doctors to spot the emergence of dangerous mutations and alter treatments before they drive the disease into more aggressive forms.
The study, based on complex genetic analysis of biopsies and blood samples from 16 patients with advanced prostate cancer, shows that treatments can act as an evolutionary force on the population of cancer cells in a tumour.
Researchers were looking in particular for clues that glucocorticoids could favour the survival of cells containing androgen receptor mutations – affecting how cells respond to hormones. They used repeat biopsies from tumours and analysed circulating tumour DNA over time, monitoring the emergence of cancer cell clones containing each mutation.
In several patients, use of glucocorticoids coincided with the emergence of androgen receptor mutations and the progression of cancer into more advanced forms.
The study also showed that measuring circulating tumour DNA levels – which is less expensive and invasive than taking repeated samples of tumours with needle biopsies – could be used to monitor the emergence of treatment-resistant prostate cancer.
Study leader Dr Gerhardt Attard, Cancer Research UK Clinician Scientist at The Institute of Cancer Research, London, and Honorary Consultant at The Royal Marsden NHS Foundation Trust, said:
“Our study showed that a steroid treatment given to patients with advanced prostate cancer and often initially very effective started to activate harmful mutations and coincided with the cancer starting to grow again.”
“Our results introduce a new paradigm for the management of patients with advanced prostate cancer. In the future, we hope to routinely monitor genetic mutations in patients with advanced disease using just a blood test – enabling us to stop treatments when they become disease drivers and select the next best treatment option. We need to confirm these findings in larger numbers of patients but using these types of blood tests could allow true personalisation of treatment for prostate cancer patients, based on the cancer mutations we detect.”
Professor Paul Workman, Interim Chief Executive at The Institute of Cancer Research, London, said:
“Drug resistance is the single biggest challenge we face in cancer research and treatment, and we are just beginning to understand how its development is driven by evolutionary pressures on tumours. This important discovery reveals how some cancer treatments can actually favour the survival of the nastiest cancer cells, and sets out the rationale for repeated monitoring of patients using blood tests, in order to track and intervene in the evolution of their cancers.”
Dr Matthew Hobbs, Deputy Director of Research at Prostate Cancer UK, said: “There are currently too few treatment options for men living with advanced stage prostate cancer. Not only do we desperately need to find more treatments for this group of men, we also need to understand more about when those that are available stop working and why. This research is important as it shows that there might be a new way to monitor how a man’s cancer is changing during treatment and that could help us to pinpoint the stage at which some drugs stop being effective. In the future this could arm doctors with the knowledge they need to ensure that no time is wasted between a drug that stops working for a man and him moving on to another effective treatment.
“However, this is an early piece of research, carried out in very few men. We now need to see this tested in a bigger group of men to establish its true potential. Anyone currently taking medication for advanced prostate cancer should not stop doing so as a result of these findings, but should speak to their clinician or a Prostate Cancer UK Specialist Nurse if they have any concerns.”
Nell Barrie, Science Information Manager at Cancer Research UK, said: “It’s vital to understand the genetic twists and turns that offer tumour cells an escape route to become resistant to treatment. And this study provides an important first step towards working out how to use tumour DNA from blood samples as a way to monitor how prostate cancer evolves during treatment.
“Cancer Research UK scientists have played an important role in unravelling how groups of cancer cells can be genetically distinct, even within the same tumour. And these latest findings shed more light on how tumours evolve.”
--ENDS--
Notes to editors
For more information please contact the ICR press office on 020 7153 5380 / [email protected]. For enquiries out of office hours, please call 07708 516357.