When we pick up our smart phone and take a photo or video and share with our friends and family, most of us do not give a second thought about the technology we’re using. We owe this modern day given to something called a complementary metal-oxide-semiconductor (CMOS) sensor, also known as the active pixel sensor (APS). It’s this type of image sensor which is used in many consumer devices, such as smart phones and webcams.
Here at The Institute of Cancer Research, London, our researchers have taken CMOS APS technology and are using it not to send snapshots, but to more effectively direct beams of radiation during cancer treatment. We’re using the technology to monitor a state-of-the-art radiotherapy technique called volumetric arc therapy (V-MAT). Generally, radiotherapy uses X-rays to deliver a treatment dose of radiation to the patient, but V-MAT delivers radiotherapy in a more complex manner. It can vary the shape of the beam, brightness and speed of rotation, speeding up treatment time and reducing radiation dose to some normal tissues. As the techniques for delivering radiotherapy develop and become more complex, the requirements for monitoring and verifying where to direct the radiation beam become ever more challenging.
CMOS APS sensors produce images more quickly, and are more sensitive, than the technologies currently used with radiotherapy, making them ideal candidates for V-MAT verification. CMOS APSs used in managing V-MAT have been modified from the model you would find in an average smart phone or webcam. Firstly, they are developed to be used safely with the ionising radiation we use in medicine – such as high-energy X-rays and proton therapy beams. Secondly, they are made using cutting-edge fabrication techniques that use more of the silicon wafer from which they are made. This means they can be made large enough to image the human body. Thirdly, the active pixel feature captures intelligence on the sensor which in turn allows manipulation of the data, such as reading out small regions of interest (ROIs) at a very fast rate, which is useful for tracking dynamic radiation treatments, such as V-MAT.
These large area CMOS detectors are the first of their kind. Work recently published by the ICR Radiotherapy Physics team has shown that these detectors can be operated at speeds of up to 400 frames per second and can accurately monitor the dose and spatial distribution of V-MAT treatments fields.
Scientists from the ICR, University of Lincoln and University of Surrey have now designed and manufactured the next generation of CMOS APSs. DynAMITe – the world’s biggest radiation-hard microchip – is one such CMOS, and measures 12.8 cm2 (200 times larger than the processing chips in a laptop). Even though it is wafer thin, DynAMITe is extremely powerful and can detect features of differing brightness at the same time and track features moving independently. The chip can also withstand very high levels of exposure to X-rays and other radiation found in medical imaging, giving it a distinct advantage over conventional detectors.
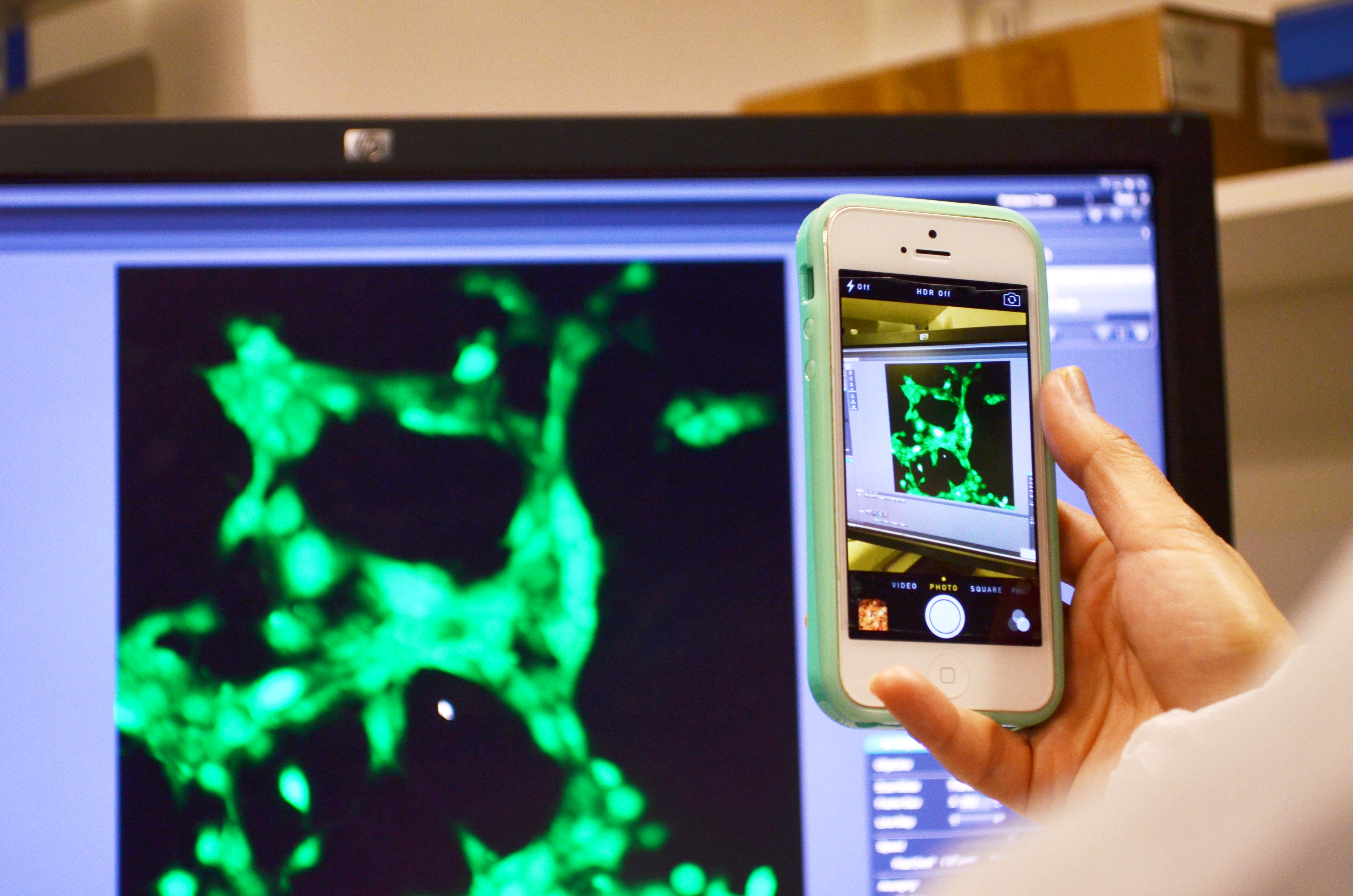
Collaborations led by Dr Emma Harris – Team Leader in Imaging for Radiotherapy Adaptation – are now applying DynAMITe in numerous applications. The chip is being tested for monitoring proton radiotherapy – a new emerging type of radiation therapy that uses charged particles to treat cancer rather than X-rays – with Professor Phil Evans at the University of Surrey and Professor Nigel Allinson, at the University of Lincoln. Research into using DynAMITe for biomedical applications is also being carried out at the University of Surrey where Dr Kevin Wells is using the device to take images of tissue samples and image fluorescence important for protein sequencing.
By working together with researchers across the UK, the ICR is changing the way we deliver and monitor radiotherapy. DynAMITe will allow the effective monitoring of radiotherapy delivery, allowing doctors to diagnose cancer and see the impact of radiotherapy treatment far more precisely than ever before. So the next time you take a photo on your smart phone, just take a moment to think about the technology that makes it possible – and the way it is being used to transform radiotherapy for patients with cancer.
Further reading:
- Zin H, Harris E, Osmond J et al. (2013). Towards real-time VMAT verification using a prototype, high-speed CMOS active pixel sensor.Phys Med Biol; 58: 3359-75.
- Esposito M, Anaxagoras T, Fant A et al. (2011). DynAMITe: A wafer scale sensor for biomedical applications. J Instrum; 6: 1-12.