August 2015
Blood test predicts cancer relapse
A blood test for breast cancer could identify which patients will suffer a relapse after treatment, months before tumours are visible on hospital scans.
Dr Nicholas Turner and colleagues at the The Institute of Cancer Research, London and The Royal Marsden devised the test to assess cancer DNA in the bloodstream as a way of tracking a small number of residual cells that had resisted treatment.
The team took tumour and blood samples from breast cancer patients with early-stage disease who had received chemotherapy followed by surgery, and who had potentially been cured of their disease.
By monitoring patients with blood tests taken after surgery and then every six months in follow-up, the researchers were able to predict who would suffer a relapse.
Women who tested positive for circulating tumour DNA were at 12 times the risk of relapse of those who tested negative, and the return of their cancer was detected an average of 7.9 months before any visible signs emerged.
The study, published in Science Translational Medicine, is an important step towards use of ‘liquid biopsies’ to revolutionise breast cancer care.
The research received funding from the NIHR Biomedical Research Centre at The Royal Marsden and the ICR, Breast Cancer Now and Cancer Research UK.
October 2015
New chemical tool to understand the role of key cancer proteins
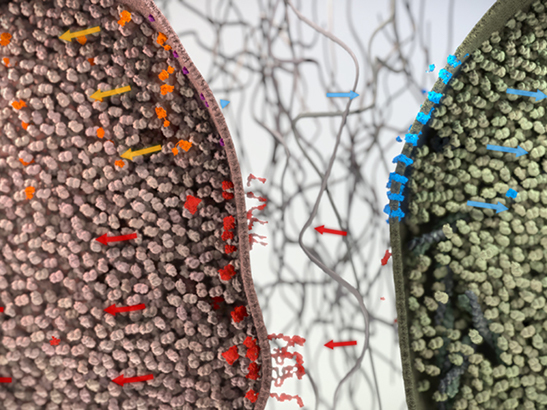
A bioassay (Jan Chlebik/the ICR)
Our scientists discovered a chemical tool which can switch off two important proteins implicated in cancer – the Mediator complex-associated kinases CDK8 and CDK19 - allowing us to fully explore their role in the disease.
Researchers led by The Institute of Cancer Research, London's Professor Julian Blagg discovered a small molecule that inhibited a cell signalling pathway known to be involved in many bowel cancers; however, at the time of its discovery they didn’t know how it was working.
In this later study, published in Nature Chemical Biology, the ICR team, in close collaboration with scientists at the University of Cardiff and Merck KGaA, Darmstadt, discovered that the chemical works by blocking two proteins called CDK8 and CDK19 which can regulate the way genes are expressed in cancer.
Using techniques such as protein crystallography, the team were able to visualise the small molecule bound to CDK8. They also examined its anticancer effects in human cancer cells lines and in mice.
Discovering and fully characterising such tools enables more detailed analysis of the roles of CDK8 and CDK19 and may shed new light on an important pathway in cancer.
This work was funded by Cancer Research UK.
October 2015
Precision drug against inherited mutations treats prostate cancer
Immunofluorescence staining showing extension of prostatic adenocarcinoma into the bladder wall in a castration resistant prostate cancer patient (Mateus Crespo/Professor Johann de Bono, the ICR)
Precision cancer treatment took another leap forward as researchers showed that olaparib, a drug licensed for women with inherited forms of ovarian cancer, can also benefit a third of men with advanced prostate cancer.
Olaparib was the world’s first drug targeting inherited cancer mutations to reach the market – licensed for women with ovarian cancer and inherited BRCA mutations. Researchers at the ICR and The Royal Marsden evaluated the drug in prostate cancer in the TOPARP-A study, and found it benefited 16 out of 49 men with advanced disease. Researchers discovered it arrested prostate cancer growth, reduced prostate specific antigen (PSA) levels and lowered circulating tumour cell counts in the blood.
Overall, a third of the men’s tumours were found to have defects in DNA repair genes, and almost 90% of these men responded well to olaparib. Men in the trial had life-limiting prostate cancer yet many went on to experience far better control of their disease than would have been expected.
A second trial, TOPARP-B, plans to give olaparib only to men with detectable DNA repair mutations in their cancers. Study leader Professor Johann de Bono, Head of Drug Development at the ICR and The Royal Marsden, says: “I hope it won’t be long before we are using olaparib in the clinic to treat prostate cancer, or before genomic stratification of cancers becomes a standard in this and other cancers.”
December 2015
Molecule helps cancer cells survive stress
A breast cancer cell (photo: National Cancer Institute)
Scientists at The Institute of Cancer Research, London discovered a chemical sensor within cancer cells that helps them override the normal stress response and allows them to survive.
The team of researchers – led by Dr Alessandro Vannini – discovered how a molecule called Brf2, levels of which are increased in some cancers, acts as a chemical sensor and shuts down gene activity when normal cells are placed under stress.
The researchers used X-ray crystallography to scrutinise the three-dimensional structure of Brf2 when the protein was in the act of recognising specific DNA sequences. The researchers think that cancer cells can overcome the trigger for cell death by producing more Brf2, allowing them to survive and accumulate mutations, even when they are under significant stress.
The molecule appears to play a key role in breast and lung cancers, and could be a promising target for future cancer drugs.
The study was published in Cell and was funded by the ICR itself, with additional support from the Biotechnology and Biological Sciences Research Council.
January 2016
Laws of nature predict cancer evolution
Intriguing research by scientists at The Institute of Cancer Research, London and Queen Mary University of London found that cancers evolve over time in patterns governed by the same natural laws that drive the flow of rivers or the brightness of stars.
The team of researchers – co-led by Dr Andrea Sottoriva at the ICR – found that many cancer types accumulated mutations in a pattern set out by a theoretical model using a so-called 1/𝑓 power-law distribution.
This pattern is found throughout nature in a variety of physical, chemical and biological systems – and even helps to govern the financial market.
The researchers believe that in the future they could predict how a cancer will grow and develop by applying these natural laws to genetic snapshots taken from a tumour.
This raises the possibility that doctors could take clinical decisions on how an individual patient’s cancer will change, and what treatments should be used, by applying mathematical formulae to tumour biopsies.
The study, published in Nature Genetics, was funded by a donation to the ICR by Chris Rokos and by organisations including Wellcome, Cancer Research UK and the Medical Research Council.
April 2016
Tumour mutation ‘corrupts’ neighbouring healthy tissue
Scientists at the The Institute of Cancer Research, London discovered that tumours can persuade nearby health cells to release unique growth signals, which cancer cells can use to multiply but cannot secrete themselves.
Published in the journal Cell, the new research sheds light on how cancer cells and normal cells communicate with each other, and could open up new approaches to cancer treatment.
Dr Chris Tape and colleagues at the ICR and Cancer Research UK Manchester Institute found that faulty versions of the KRAS gene – often mutated in cancer – can have an important effect on healthy stromal tissue.
Normal KRAS makes occasional signals that tell a cell to divide, but when mutated the gene becomes hyperactive and helps drive cancer cells’ rapid and uncontrolled growth.
By monitoring proteins in an abnormal cell and a healthy neighbouring cell at the same time, they discovered that healthy cells were responding with a new message that doubled the capacity for KRAS to drive malignant behaviour in the cancer cells.
The study showed for the first time that there is a communication loop with a cancer-causing gene controlling tumour growth via healthy stromal cells.
This work was funded by the Wellcome Trust, Cancer Research UK and the Rosetrees Trust.
May 2016
New resistance-busting cancer drug discovered
Scientists at The Institute of Cancer Research, London discovered a potent new cancer drug that has progressed into clinical trials.
Professor Ian Collins led a team of scientists who worked in partnership with colleagues at the drug discovery company Sareum to discover the drug, known as CCT245737, which blocks an important molecule called CHK1.
Most chemotherapies work by damaging the DNA of rapidly dividing cells. But in response, cancer cells activate CHK1 which delays cell division and gives cancer cells time to repair their damaged DNA. Researchers have been trying to work out how best to target this molecule and prevent cancers from resisting treatment.
The researchers used a variety of different assays to identify the most potent, selective and orally available drug that targets the CHK1 molecule.
When tested in mice with tumours grown from human cell lines, the drug was found to be effective as a single oral dose, which is an important indicator that it could be clinically effective, particularly as many of the CHK1 inhibitors currently studied are intra-venous only.
The research was published in the Journal of Medicinal Chemistry. The drug, which has now been progressed into clinical trials, was designed and synthesised at the ICR with funding from Cancer Research UK.
June 2016
Lung cancer can be treated using UK's first MR Linac radiotherapy
Researchers at The Institute of Cancer Research, London and The Royal Marsden NHS Foundation Trust have shown that lung cancer could be treated using their state-of-the-art new MR Linac radiotherapy machine.
The new MR Linac, the first installed in the UK, combines an MRI scanner with a sophisticated radiotherapy system to precisely locate tumours and adjust radiation beams in real time.
The magnetic field used by MRI distorts the radiation dose within the patient delivered by radiotherapy, particularly at points where air and tissue meet like in the lungs. The impact of these effects for dose distributions in the lung was unknown.
Researchers led by the ICR’s Professor Uwe Oelfke and the Royal Marsden’s Dr Fiona McDonald showed that it is possible to design MR Linac radiotherapy treatments that meet all clinical standards, using scans from nine lung cancer patients.
The research, published in the journal Radiotherapy and Oncology, showed that MR Linac radiotherapy could potentially spare healthy tissue from radiation, by adapting the treatment beam's position to the motion caused by breathing.
The research was funded by Cancer Research UK with support from Elekta AB and the NIHR Biomedical Research Centre at The Royal Marsden and the ICR.
July 2016
New approach streamlines gene testing in ovarian cancer
Researchers at The Institute of Cancer Research, London and The Royal Marsden NHS Foundation Trust successfully piloted a streamlined approach to gene testing in women with ovarian cancer. The new approach is faster, simpler and much more cost-effective than the standard testing procedure with a potential annual saving of £2.6 million a year if adopted across the NHS.
The new procedure involves offering BRCA gene testing for women with ovarian cancer in routine cancer clinics instead of them having to be referred to clinical genetics teams. Patients found to have a BRCA mutation get an appointment with the genetics team to discuss the implications for themselves and their families in detail.
The new approach was developed by Professor Nazneen Rahman and colleagues under the Mainstreaming Cancer Genetics programme, funded by Wellcome. It has now become standard at The Royal Marsden and is being adopted by hospitals across the UK and internationally.
Details of the new testing pathway were published in the journal Scientific Reports, and the work was funded by the NIHR Biomedical Research Centre at The Royal Marsden and the ICR, and the Royal Marsden Cancer Charity.
August 2016
New radiotherapy regime could save NHS tens of millions per year
Intensity modulated radiation therapy machine (photo: Jan Chlebik/the ICR)
A shorter course of prostate cancer radiotherapy, involving fewer hospital visits, is as effective for maintaining patients’ survival and quality of life as standard treatment.
This was shown in a 14-year trial led by researchers at The Institute of Cancer Research, London and The Royal Marsden NHS Foundation Trust and published in The Lancet Oncology.
The researchers found benefits for a 20-dose course of a modern type of radiotherapy over a 37-dose course, which is the current NHS standard.
The new regime would save 17 hospital trips and complex radiotherapy treatments for each patient, leading to a reduction nationally of more than 150,000 visits per year.
The international trial, which recruited over 3,200 men, was funded by Cancer Research UK and the Department of Health.