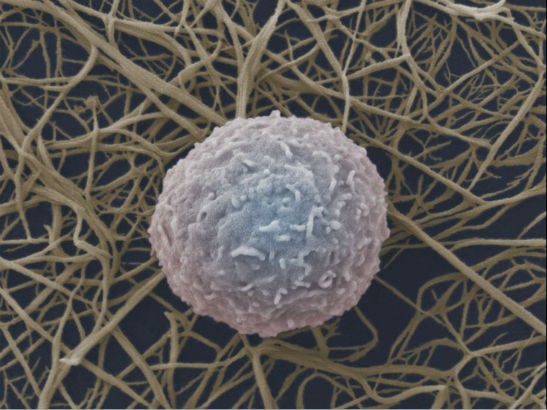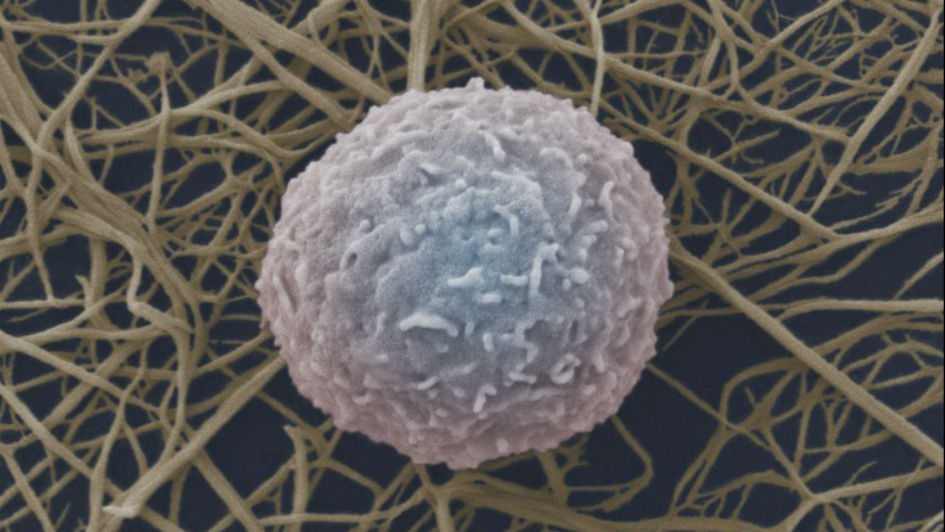
Image: white blood cell. Credit: Wellcome Images
Scientists have uncovered a promising treatment strategy for an aggressive type of leukaemia – through targeting the enzymes that cells normally use to sense and adapt to changing oxygen levels.
In findings published in Nature Cancer, researchers revealed that blocking these oxygen-sensing enzymes can significantly halt acute myeloid leukaemia in mice and patient samples without affecting normal production of blood cells.
Existing drugs to treat anaemia could be used for AML
The enzymes can already be blocked safely with existing drugs used to treat anaemia, so the researchers hope to see their findings translated to clinical trials for leukaemia.
Excitingly, the team has also developed a new first-in-class drug which more selectively blocks the enzymes than existing drugs, and so may reduce side effects.
The research was funded by Cancer Research UK, Medical Research Council and Barts Charity.
Current treatments for AML have toxic side effects
Acute myeloid leukaemia (AML) is an aggressive type of blood cancer that usually affects older adults but also occurs in children and young adults. In AML, patients experience a dramatically increased production of immature white blood cells (called blasts), which is driven by mutations in the stem and progenitor cells that usually give rise to normal blood cells. These blasts in turn damage the bone marrow and other organs with devastating consequences to the patients.
There are few treatment options for AML, and therapies have remained relatively unchanged for the last 30 years, with the majority of patients receiving chemotherapy and bone marrow transplants to control their condition. Unfortunately, many of these treatments are not effective and they cause toxic side effects.
Targeting how cells sense oxygen levels
The research was co-led by scientists from The Institute of Cancer Research, London, and the University of Oxford, and partly undertaken at Queen Mary University of London.
The work aimed to understand whether enzymes called hypoxia-inducible factor prolyl hydroxylases (PHDs) – which sense levels of oxygen in the body – could be a drug target for treating acute myeloid leukaemia.
In the presence of oxygen, the PHD enzymes are active and target hypoxia-inducible factor (HIF) proteins for their destruction. Under hypoxia – when oxygen levels are low – PHD enzymes are less active resulting in increased levels of HIF.
Boosting levels of HIF could treat AML
The team had previously shown that inactivation of HIF promotes aggressive AML, and now they set out to uncover whether boosting the levels of HIF could prevent AML progression. In this study, they achieved this by blocking or genetically inactivating PHDs.
In studies in mice, they showed that genetic modification to inactivate PHD enzymes increased HIF levels and stopped leukaemia from starting or progressing, without affecting the normal production of blood cells.
They showed the same anti-leukaemia effect by inactivating PHD using existing drugs currently used to treat anaemia – in mouse cells and patient samples.
Notably, they generated a new first-in-class PHD inhibitor called IOX5, which selectively inhibits PHDs, without inactivating any other enzymes. They found that IOX5 significantly blocked AML progression. The anti-cancer effect of IOX5 was further increased when combined with Venetoclax, a drug used to treat various types of leukaemia.
The findings provide a ‘proof-of-concept’ that blocking PHD enzymes is an effective strategy against acute myeloid leukaemia.
'A new way to treat leukaemia'
Professor Kamil Kranc, Professor of Haemato-Oncology at The Institute of Cancer Research, London, said:
“Therapy for acute myeloid leukaemia has barely changed in several decades. There is a huge need to discover better treatments for this aggressive disease. We’ve shown for the first time that targeting the pathways that our cells use to respond to oxygen levels could provide a new way to treat leukaemia, without impacting the normal production of blood cells within the bone marrow. Dr Hannah Lawson in my laboratory played a critical role in discovering PHDs as therapeutic targets in AML and conducting leukaemia biology experiments.
“Our next challenge is to progress the existing drugs and our new, more selective compound, to clinical trials. We’re hopeful this research will pave the way towards a new era of AML treatments, and we’d like to explore whether these therapies could also be beneficial for solid tumours.”
Professor Christopher Schofield, study co-leader and Professor of Chemistry at the University of Oxford, said:
“This finding is the outcome of many years of collaborative research, between Oxford’s chemistry and biochemistry group where Dr James Holt-Martyn played a key role, and the Institute of Cancer Research’s biology group. Previously, our group worked with Professor Sir Peter Ratcliffe on his Nobel Prize-winning research, a collaboration which enabled the development of clinically used PHD inhibitors to treat anaemia. We’re extremely excited to now find that the same PHD targets have potential for the treatment of leukaemia.”
Professor Kristian Helin, Chief Executive Officer at The Institute of Cancer Research, London, said:
“Cancer exists in a complex ecosystem within the body. This work provides important insights into that ecosystem, and the way in which cancer uses signals within the environment – such as those relating to oxygen levels – to grow and develop. This study is also an excellent example of cancer researchers and chemists working closely together to develop and test new cancer therapeutics.
“It’s exciting to see how a concept develops through a fundamental discovery project and the development of a first-in-class small molecule inhibitor, to potentially benefiting patients with this devastating type of cancer, and I look forward to seeing this research progress into clinical trials.”