Scientists at The Institute of Cancer Research, London, have found a way to identify people with inflammatory bowel disease (IBD) who are at the highest risk of developing bowel cancer.
IBD includes ulcerative colitis and Crohn’s disease. They irritate the lining of the bowel, which can cause abnormal pre-cancerous cells to form if left untreated. Having these conditions can increase your risk of bowel cancer, especially if you have had them for several years. According to the charity Crohn’s and Colitis UK, one in 123 (around 500,000 people) in the UK have Crohn’s disease or ulcerative colitis.
Identifying the people more likely to develop bowel cancer
In a study published today in the journal Gut, scientists at The Institute of Cancer Research (ICR), funded by Cancer Research UK and the Barts Charity and working with doctors at St Mark’s Hospital, the UK’s specialist bowel hospital, revealed that people with IBD whose pre-cancerous cells had lost or gained multiple copies of their DNA were far more likely to go on to develop bowel cancer. The scientists created an algorithm that calculates the risk of future bowel cancer, based on the exact pattern of the DNA altered in the pre-cancerous cells.
The scientists found that this method can predict which people with IBD who develop pre-cancerous cells will go on to develop bowel cancer within 5 years with greater than 90% accuracy. This method could be used in hospitals to test for bowel cancer risk in people with IBD in the coming years.
Sparing those who are not at high risk from tough decisions
Professor Trevor Graham, Professor of Genomics and Evolution and Director of the Centre for Evolution and Cancer at The Institute of Cancer Research, London, said:
“Most people with ulcerative colitis or Crohn’s disease won’t develop bowel cancer. But for those that have these conditions and are showing signs of pre-cancer in their colon, there are some tough decisions to make. Either they have it monitored regularly, in the hope that it doesn’t become cancer, or they have their bowel removed to guarantee they don’t get cancer in the future. Neither of these options are particularly pleasant.
“Crohn’s and ulcerative colitis are common and we need better tools to identify the patients at highest risk of bowel cancer. Our test and algorithm give people with IBD, and the doctors who care for them, the best possible information so that they can make the right decision about how to manage their cancer risk. We can accurately identify those people at high risk whilst putting the minds of many others at rest.”
Algorithm calculates risk
The test would use genomic sequencing to check the number of copies of DNA from samples of pre-cancerous growths taken from the lining of the gut during endoscopy. Information from the sequencing would be fed into an algorithm, which calculates their risk based on which copies of DNA are altered, alongside other information such as the size of the growth, how easy it was to remove during biopsy and how inflamed the gut is overall.
Currently, people with IBD are offered regular checks for pre-cancerous growths in the lining of the gut. People with the pre-cancerous growths (known as low grade dysplasia or LGD) have around a 30% chance of bowel cancer developing over 10 years. If the patient has LGD, they are classed as high risk and offered treatment to prevent the pre-cancerous cells developing into bowel cancer.
The treatments are bowel removal surgery, which has life-changing side effects such as carrying a stoma bag, or regular monitoring with colonoscopies, which are invasive, time-consuming and cause worry and anxiety for patients because they live with the fear that they may develop bowel cancer in the future.
Craig Foster, from Waterlooville, lost his wife Fariba to bowel cancer in February 2024.

Fariba, who worked as a dental receptionist, had lived with ulcerative colitis since she was 18, when she had three-quarters of her bowel removed. Craig said:
“Cancer takes no prisoners and it doesn’t matter who you are or from what walk of life, everyone is affected in some way. Fariba died just six months after she was diagnosed. Even though it was a short time, it was the worst time.
“Research like this will save lives. It gives me comfort to know that there are scientists working right now so that no-one has to experience the same situation Fariba was in.”
The only way to find these pre-cancerous cells is through biopsy, but it does not reliably tell doctors which pre-cancers will eventually become bowel cancer. Scientists hope that the test could spare those who are at much lower risk from the stress of regular colonoscopies or the life-changing impact of surgery to remove the colon.
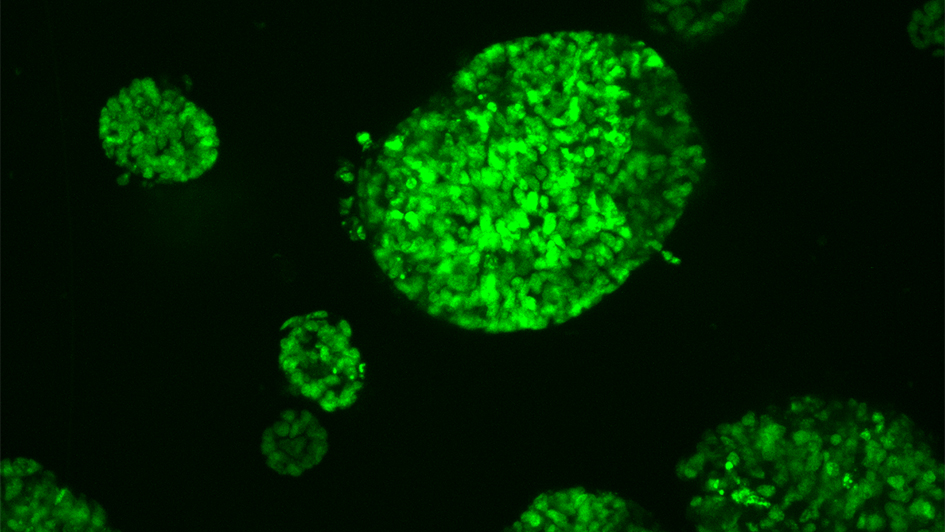
In the study, samples of pre-cancerous cells were taken from 122 patients with IBD. Around half of the patients subsequently went on to develop bowel cancer 5 years after the sample was taken, whilst the other half remained cancer-free after 5 years. All of the samples had their full DNA scanned to look for changes in the structure and number of copies in the DNA. The scientists found that patients with IBD who developed bowel cancer had lost multiple copies of their DNA.
In future studies, the scientists are hoping to develop the test beyond analysing samples of growths taken from the gut to a less invasive method, such as taking a blood sample.
‘Finding smarter ways to assess these colons is much needed’
Professor Ailsa Hart, Lead of the inflammatory bowel disease research unit at St Mark’s the National Bowel Hospital and co-lead of the study, said:
"Patients with inflammatory bowel disease have a higher risk of developing colorectal cancer than people without IBD, and need to undergo assessment with regular colonoscopies to try to detect early signs of cancer. These tests are onerous and unpleasant for patients, imperfect at detecting early cancer changes and costly to health services.
“If early signs of cancer are detected, surgery, which involves removing the colon, is advocated. Finding smarter ways to assess these colons is much needed.
“Here we describe a potential biomarker, which can be readily translated into clinical practice, to improve assessment of patients with IBD and early signs of cancer to help with the decision for surgery.”
‘Until now we have had to take a one-size-fits-all approach’
Dr Ian Foulkes, Executive Director of Research and Innovation at Cancer Research UK, said:
“Treatment for bowel cancer is far more likely to be effective if you catch the disease earlier. Having Crohn’s or colitis is a known risk for bowel cancer but the risk varies widely between different people, and until now we have had to take a one-size-fits-all approach to preventing it.
“Genome sequencing is now far cheaper and more widespread than ever before, and it’s changing how we look at cancer. Getting a full readout of tumour DNA means we can see a much bigger picture of how someone’s cancer started and how it is likely to change over time.
“With this research, we can focus resources on treating people with IBD who are at really high risk, saving health services valuable time and money. We can also give those at lower risk peace of mind and remove the fear of bowel cancer in the future.”