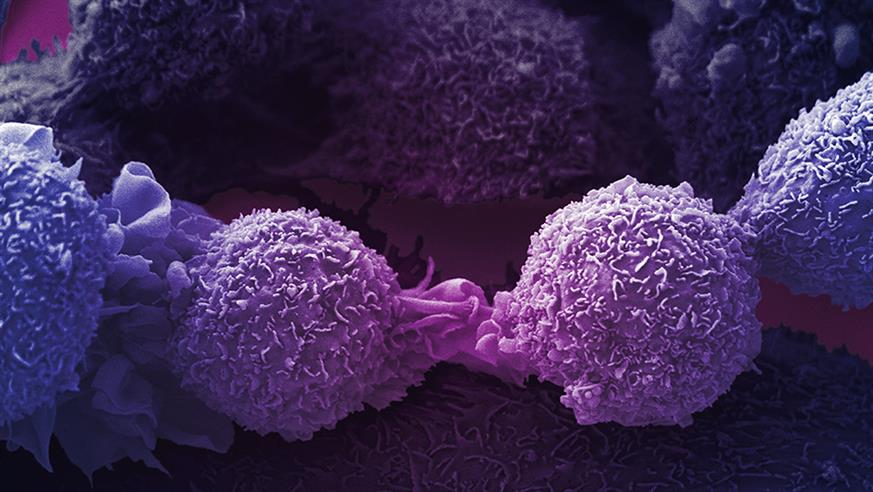
Image: Lung cancer cells courtesy of the Wellcome Collection. License: CC BY-NC 4.0
Scientists discovered that when the breast cancer drug palbociclib was combined with the lung cancer drug crizotinib, the two-drug combination was significantly more effective against cancer cells in the laboratory than either drug used on its own.
Palbociclib has been described as one of the biggest advances in women with advanced breast cancer for two decades – so the prospect of being able to make the treatment even more effective is exciting.
The new findings also suggest that the combination approach could broaden the clinical use of palbociclib – and other drugs that work in the same way – beyond breast cancer to include many other tumour types as well.
Pairing two drugs blocks resistance pathways
Scientists at The Institute of Cancer Research, London, and UCL Cancer Institute discovered that resistance to palbociclib is often driven by a protein which is targeted by crizotinib – providing the rationale for using these two drugs together.
Their new study is published today (Friday) in the journal Oncogene and was funded by Wellcome.
Palbociclib is one of a group of drugs which are currently used to treat patients with hormone receptor-positive breast cancer by blocking the function of two proteins – CDK4 and CDK6 – which promote tumour cell division and cancer progression.
However, cancers can become resistant to palbociclib by activating a related molecule called CDK2, which is able to drive cell division in the absence of CDK4/6.
Our new Centre for Cancer Drug Discovery promises to bring together unique, multi-disciplinary teams of evolutionary biologists, chemists, big data specialists and clinicians. Explore the new building floor by floor.
In the new study, the researchers found that CDK2 can compensate for inhibition of CDK4/6 in cancer cells by signalling via a cellular control pathway involving the key molecules MET and FAK.
Based on this discovery, the researchers found that pairing CDK4/6 inhibitors such as palbociclib together with crizotinib – which blocks MET activity – created a combination treatment that was much more effective than either drug on its own against cancer cells grown in the lab or human tumours growing in mice.
The combined agents acted synergistically not only to block cancer cell division but also to induce senescence – a state in which cells are thought to stop growing and dividing but without undergoing cell death.
The researchers achieved promising results in cancer cells derived from different organs in the body – from breast and lung to bowel – indicating that there is potential to expand clinical use of palbociclib and other CDK4/6 inhibitors beyond breast cancer to benefit a wider range of patients.
Identifying key molecules for resistance
To reveal the mechanism underlying the resistance, the researchers searched systematically using robotics and sophisticated imaging to identify how CDK2 is activated to allow cells to evade CDK4/6 inhibitors.
They discovered that MET and FAK were critical molecules in the signalling pathway used by cancer cells to survive and develop resistance to palbociclib treatment.
The researchers hope that their discoveries can be translated to patients – initially by evaluating the safety and effectiveness of combining CDK4/6 inhibitors like palbociclib with MET inhibitors such as crizotinib.
It may be possible to develop lab tests to identify which patients would benefit from the use of the crizotinib in this way.
Such tests would need to cover the various ways that MET itself can be important – involving events in the cancer cells themselves and also contributions from surrounding host cells within the microenvironment of the tumour.
And looking a little further into the future, the researchers also highlight the possibility arising from their research that combining CDK4/6 inhibitors with drugs that block FAK could be even more effective and more generally applicable.
This is because their findings show that FAK is a critical node in the cellular circuitry leading to unwanted CDK2 activation.
FAK can not only be activated by MET but also by other signalling molecules including ones from the tumour environment called integrins which are involved in cell interactions. That means combined inhibition of FAK and CDK4/6 could have broader effects extending to a wider range of cancers.
FAK inhibitors are already in clinical trials and so this idea could be tested soon.
Innovative approaches at the heart of ICR research
Combining targeted drugs with different mechanisms of action is one of the central strategies the ICR is pursuing as part of a pioneering research programme to combat the ability of cancers to adapt, evolve and become drug resistant.
The ICR – a charity and research institute – is raising the final £15 million of a £75 million investment in a new Centre for Cancer Drug Discovery to house a world-first programme of ‘anti-evolution’ therapies.
Study co-leader Professor Paul Workman, Chief Executive of The Institute of Cancer Research, London, said:
“Cancer’s ability to adapt, evolve and become drug resistant is the biggest challenge we face in creating more effective treatments for the disease. In this study, we sought to understand exactly how resistance occurs to an important family of breast cancer drugs, so that we can stay one step ahead of the cancer.
“We have shown the potential of combining two precision medicines for breast and lung cancer together to create a two-pronged attack that strips cancer cells of their resistance. We still need to do more work to understand the full potential of combination treatment to increase the effectiveness of these drugs, but the approach looks highly promising and has the potential to be effective against several cancer types.”
Study co-lead Professor Sibylle Mittnacht, Professor of Molecular Cancer Biology at UCL Cancer Institute, said:
“Our evidence shows that existing medicines could be used to overcome resistance to treatment in a frequent form of breast cancer in women.
“In addition, use of a current breast cancer medicine together with these other medicines could be a new, promising route for the treatment of lung and several other cancers.”
