Video: "Standard of care treatments follows the results of the trials that we published." Watch Professor Judith Bliss, Dr Anna Kirby and Jo Haviland talk about their work on breast cancer radiotherapy.
Improved radiotherapy approaches for breast cancer treatment
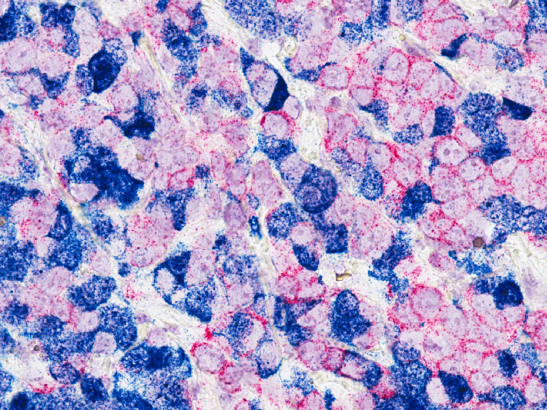
Radiotherapy is a crucial part of treatment for breast cancer, used for many of the 55,000 women who are diagnosed with the disease each year. But while radiotherapy does help save lives, it can also take a physical and emotional toll.
It can cause long-term adverse effects, for example, such as hardening or shrinking of the breast, breast discomfort and skin changes, which can have a lasting impact on patients. Other effects can also occur, albeit rarely, including lung fibrosis and heart damage.
This toxicity has become an increasingly important consideration as more women survive breast cancer and the chance of cancer returning in the affected breast is now very low – in fact, for some patients the side effects can pose more of a hazard than the risk of relapse. This makes treatment schedules that improve how we treat the breast, while keeping side-effects to a minimum, all the more necessary.
Historically, the standard radiotherapy treatment for breast cancer was to administer multiple small doses (or fractions) of radiation of no more than 2 Gray (Gy) up to 50 Gy. A five-week treatment of 50 Gy in 25 fractions was the international standard, but an analysis by the Royal College of Radiologists in the 1980s found that breast cancer radiotherapy wasn’t standardised across the UK, with considerable variation in treatment schedules, including in the size and number of fractions that we being used.
Research at the ICR, led by Professor John Yarnold, ICR Emeritus Professor of Clinical Oncology, suggested that breast cancer radiotherapy could benefit from a ‘hypofractionated’ approach of fewer, larger fractions over a shorter time period to a lower total dose.
Our scientists – including Professor Yarnold and Professor Judith Bliss, Director of the ICR’s Cancer Research UK-funded Clinical Trials and Statistics Unit (ICR-CTSU) and Team Leader of Breast and Rare Cancers Trials – have been key players in developing and initiating several clinical trials demonstrating the safety and efficacy of a hypofractionated approach.
Professor Bliss says: “It was always going to be of interest to see if we could give the biological equivalent total dose of radiotherapy, which quantifies the expected biological effect, in a shorter number of individual doses to ease the burden on the patient. But to do that, you have to get the total dose and dose per fraction right – if you don’t make the right adjustments then that can lead you to nasty side-effects.”
Hypofractionation from the start
Based on these factors, the ICR has spearheaded research spanning several decades that has investigated the use of hypofractionated radiotherapy for breast cancer. Led by Professor Bliss and Professor Yarnold, the series of Standardisation of Breast Radiotherapy (START) trials are among the most prominent studies of hypofractionation ever undertaken, playing a major role in changing clinical practice by developing new hypofractionated standards for breast cancer.
The three START trials, funded by CRUK, Medical Research Council and UK Department of Health and Social Care, recruited more than 4,000 women with completely excised invasive breast cancer, enrolled from 35 centres, to randomly receive hypofractionated or standard radiotherapy regimens.
The START-P pilot study, for which 10-year results were published in 2006, first established that radiotherapy schedules could be simplified from the standard 50 Gy in 25 fractions by delivering fewer, larger doses that didn’t compromise on cancer control or safety.
As a follow-on to START-P, the START-A trial investigated two alternative test doses of hypofractionated radiotherapy in shorter 13-fraction schedules of 41.6 Gy and 39 Gy, compared with 50 Gy, all administered over five weeks.
Meanwhile, the START-B trial examined the effect of delivering 40 Gy in 15 fractions over a shorter schedule of three weeks. START-B confirmed the hypofractionated schedule was as effective as 50 Gy in 25 fractions, with the estimated five-year local relapse risk for patients standing at 3.8 per cent for the former versus 5.2 per cent for the latter.
As a result of these findings, the National Institute for Health and Care Excellence recommended the 40 Gy in 15 fractions regimen as a standard of care for in the UK in 2009. This regimen was estimated to treat 25,000 women per year for their breast cancer – amounting to a saving of £240 million annually for the NHS, while making up 92 per cent of weekly courses in adjuvant breast cancer radiotherapy.
The uptake of the 40 Gy regimen has saved each patient an estimated 14 hours in travel and appointment time – a total of more than 345,000 hours each year for all patients – with women reporting fewer late tissue damage effects, such as breast shrinkage, than the 50 Gy regimen.
Internationally, bodies including the American Society for Radiation Oncology and the European Society for Radiotherapy have endorsed the START-B regimen, leading to increased uptake around the world and helping to shape international practice.
Professor Bliss says: “The START trials were based on ascertaining the most efficient way to deliver radiotherapy for breast cancer so that disease control is at least as good as the previous standard of care. The balance is always about making sure patients remain safe while still maintaining the same level of efficacy.”
FAST-Forward
Building on the START trials and using the same type of three-group trial design, Professor Bliss, along with other statisticians and clinicians at the ICR, and Professor Yarnold (before the role of clinical lead was taken over by Professor Murray Brunt at Keele University) developed the NIHR FAST-Forward trial. This trial was set up to investigate whether hypofractionation could be taken further, streamlining the way radiotherapy was delivered to improve efficiency without compromising on safety.
FAST-Forward compared the 40 Gy regimen, which by now had become standard across the UK, with a lower total dose of 26 Gy or 27 Gy given in five fractions over just one week. Compared to the five and three-week regimens of the START trials, these experimental schedules would significantly cut down treatment times for patients.
In 2020, FAST-Forward’s five-year results confirmed that the 26 Gy regimen was as good at controlling the cancer as the 40 Gy one with no significant increase in side effects, leading to another change of standard practice as this shorter schedule was rapidly adopted.
The findings of FAST-Forward were especially significant amid the Covid-19 pandemic, as they enabled the NHS to cut down patient visits to hospital for treatment from 15 to five – reducing the risk of infection, as well as saving the NHS a projected £40 million a year.
Crucially, the streamlined schedule has also allowed treatments to continue during the pandemic because it has been more manageable for the NHS at a time of extreme pressure on workloads, infrastructure and resources.
An international panel of experts recommended 26 Gy in five fractions as an emergency treatment for immediate adoption in May 2020, its use increasing from less than 0.2 per cent to 60 per cent between April 2019 and April 2020. It was incorporated into the Royal College of Radiologists national consensus guidelines in October 2020.
Jo Haviland, a Principal Statistician at the ICR-CTSU, who led the statistical analysis of both the START and FAST-Forward trials, says:
“We expanded on what we found in the START trials to establish that 15 fractions isn’t the limit – we can extend it even further to five. It has always been about looking at how we can still cure the cancer and keep recurrence rates down, but without causing more side effects. By determining the trade-off between these two aspects, we have been able to make treatments significantly more convenient and tolerable for patients.”
The REF is the UK’s system for the assessment of research quality and impact at its higher education institutions. To mark our outstanding success, we are celebrating some of the ICR research programmes that have been changing the lives of cancer patients.
Read more about REF2021
Partial or whole breast radiation
Optimising the delivery of radiotherapy doesn’t stop at hypofractionation. Radiotherapy is usually received by patients after they have undergone breast conserving surgery, which is known to reduce the risk of relapse. Irradiation tends to be to the whole breast and most patients receive this treatment, regardless of their risk of relapse.
But by the 2010s, researchers at the ICR were reasoning that if radiotherapy could be restricted to only the parts of the breast where the cancer had previously been located and where the patient is most likely to experience disease recurrence, it may help to reduce side effects, especially in low-risk patients who may be being overtreated.
That was the rationale for the multicentre, CRUK-funded IMPORT LOW trial, which compared partial-breast with whole-breast radiotherapy in women with breast cancer with a low risk of relapse. Professor Yarnold was the clinical lead for the trial before being replaced by Professor Charlotte Coles at the University of Cambridge.
The trial, for which Professor Bliss was the ICR’s scientific lead, investigated the use of partial-breast radiotherapy in 40 Gy in 15 fractions over three weeks in more than 2,000 patients. It found that targeting radiotherapy to only the tumour-excised areas was as effective at controlling the cancer at five years as whole-breast radiation.
Further analysis also established that more than half of patients didn’t report any marked or moderate side effects, with most effects diminishing over time. The trial also helped to facilitate the development of 3D intensity modulated radiotherapy (IMRT) across the UK, which allows for more accurate targeting of the cancer by shaping the radiation beam to match the contours of tumours.
Minimising disease burden
Professor Bliss says: “The rationale behind all of these trials was that if it was possible, it is always preferable to develop a treatment schedule that minimises the burden on the patient, so they are not being treated unnecessarily and don’t need to come in for treatment on as many occasions.
“The biggest gain that has been made is in terms of reducing treatment times – first from five weeks to three and now just one week, which has had a substantial impact on patients’ lives and healthcare practices, as shown by its widespread use in the UK and rapid adoption internationally. This has also helped to make radiotherapy more accessible to more women, such as those who are older or live in lower-income countries, and who may be disadvantaged by frequent hospital visits.
“The START, FAST-Forward and IMPORT LOW trials have each propelled breast cancer radiotherapy to a new standard that has transformed how we treat patients, and it is fantastic to see all the progress we have made in this area to the benefit of so many.”