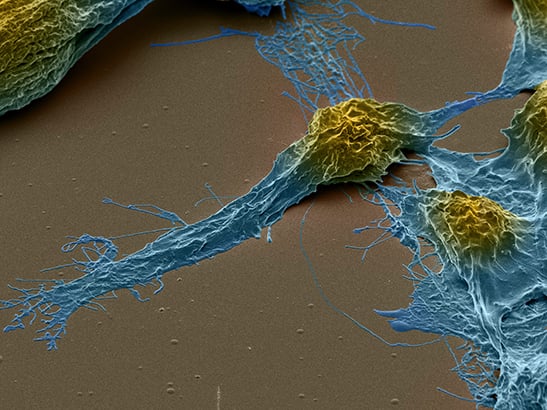
Highly invasive human paediatric brain tumour derived cells. Image courtesy of Professor Chris Jones.
A new type of drug that targets a genetic weakness in an untreatable childhood brain cancer could become the first ever treatment designed to target the disease.
The prototype treatment could also offer hope for patients with the rare and devastating ‘stone man syndrome’ – in which muscles and ligaments turn to bone.
Scientists at The Institute of Cancer Research, London, led research with an international team of colleagues, finding that the new drug class can kill brain cancer cells with mutations in the ACVR1 gene and shrink tumours in mice.
Open science company M4K (Medicines for Kids) Pharma has taken on development of the ACVR1 inhibitor drugs – and clinical trials in children with brain cancer are expected to begin in 2021.
There have been no new drugs licensed to treat brain cancer in adults or children for 20 years.
A promising new treatment
The new type of drug targets the protein molecule produced by mutated versions of the ACVR1 gene found in the deadly childhood brain cancer ‘diffuse intrinsic pontine glioma’ (DIPG).
Curiously, ACVR1 mutations don’t exist in any other type of cancer, but they are the cause of the inherited disease, stone man syndrome, where damaged muscle remodels as bone as it heals.
The study is published in the journal Communications Biology today and was funded by Abbie's Army, Children with Cancer UK, Cancer Research UK and the DIPG collaborative.
There are currently no life-extending treatments other than radiotherapy for DIPG tumours and this is never curative, with children expecting to live only nine to 12 months after diagnosis.
Because they occur in the brainstem or ‘pons’ area of the brain, DIPG tumours can’t be removed by surgery, and chemotherapy simply doesn’t work.
Survival extended by 25 per cent
In 2014, scientists at The Institute of Cancer Research (ICR) discovered that ACVR1 mutations occur in a quarter of DIPG tumours and have been working on drugs that target it ever since.
Following this discovery, teams at the Structural Genomics Consortium in Oxford and the ICR created a new series of molecules that target mutant forms of ACVR1.
In the new study, the ICR-led team tested 11 prototype drugs with anti-ACVR1 activity – including some from the Structural Genomics Consortium, as well as other drugs previously investigated for stone man syndrome – on brain cancer cells grown in the lab.
They found that two of the prototypes from the new series were particularly good at blocking signals sent out by ACVR1 and killing ACVR1-mutant cells, while having very little effect on healthy brain cells.
The researchers transplanted human DIPG tumours into mice and found the potential new drugs stopped ACVR1 activity, shrunk tumours and extended survival by 25 per cent (from 67 to 82 days).
The activin A connection
Looking at cells in the lab, the new study shows that ACVR1-mutant cells respond inappropriately to a molecule called activin A – which is present in high levels during brain development – sparking a cascade of events that trigger tumour growth.
A similar situation is thought to occur in stone man syndrome, with high levels of activin A occurring during inflammation in muscles and inappropriately triggering the formation of bone tissue in people born with ACVR1 mutations.
The drugs have now been taken on as the first project of a new open science company called M4K Pharma, which aims to discover and develop affordable drugs for childhood diseases that are rare, where there is less market incentive and that aren’t well served by current business models.
Professor Chris Jones, Professor of Paediatric Brain Tumour Biology at The Institute of Cancer Research, London, said:
“It’s simply not good enough that we can cure some cancers, but in others we have seen no progress in decades. We owe it to children and their families to do better.
“DIPG is a relatively rare childhood brain cancer, but it is always deadly. Learning more about the biology of DIPG, and trying to find ways to translate that knowledge into new treatments, has been a passion of mine for years. My lab discovered that mutations in the ACVR1 gene occur in a quarter of DIPG cancers and it’s incredibly exciting to see this now lead to potential new drugs for the disease. I can’t wait to see how they perform in patients.
The ICR is committed to discovering and developing cures for all childhood cancers. Support our mission.
'An important study'
Professor Paul Workman, Chief Executive of The Institute of Cancer Research, London, said:
“This is an important study which perfectly illustrates how gaining a detailed understanding of the biology of cancers can allow us to move very quickly to the discovery of new treatments — in this case to a devastating rare type of children’s brain cancer.
“I’m proud that the ICR is working in an academic-industry partnership with the biotech company M4K Pharma to take drugs forward to the clinic. Where the patient population is very small, it can be difficult to get companies to take such drugs on. And even where this does happen the result is often a very expensive drug that the NHS struggles to afford. One important solution, as shown here, is for academic researchers to take a leading role in working closely with companies to create genuinely innovative treatments at an acceptable price.
“I hope that a new drug from this research can be taken to the clinic as quickly as possible to help children with DIPG tumours, and of course it would also be excellent to see patients with stone man syndrome benefit from the treatment as well.”
Amanda and Ray Mifsud lost their six-year old daughter Abbie to DIPG brain cancer in 2011. Together they set up Abbie’s Army in November 2012 so that one day parents of children diagnosed with DIPG will not be told that there is no cure and no hope, as they were. Amanda said:
“We’re so pleased to see some of the pre-clinical research work that ‘Abbie’s Army’ has supported in the Jones lab with ACVR1 heading towards a biologically relevant treatment. Our hope very much is that further translation and combination studies will provide a successful therapy for this sub-set of DIPG patients in the near future.”