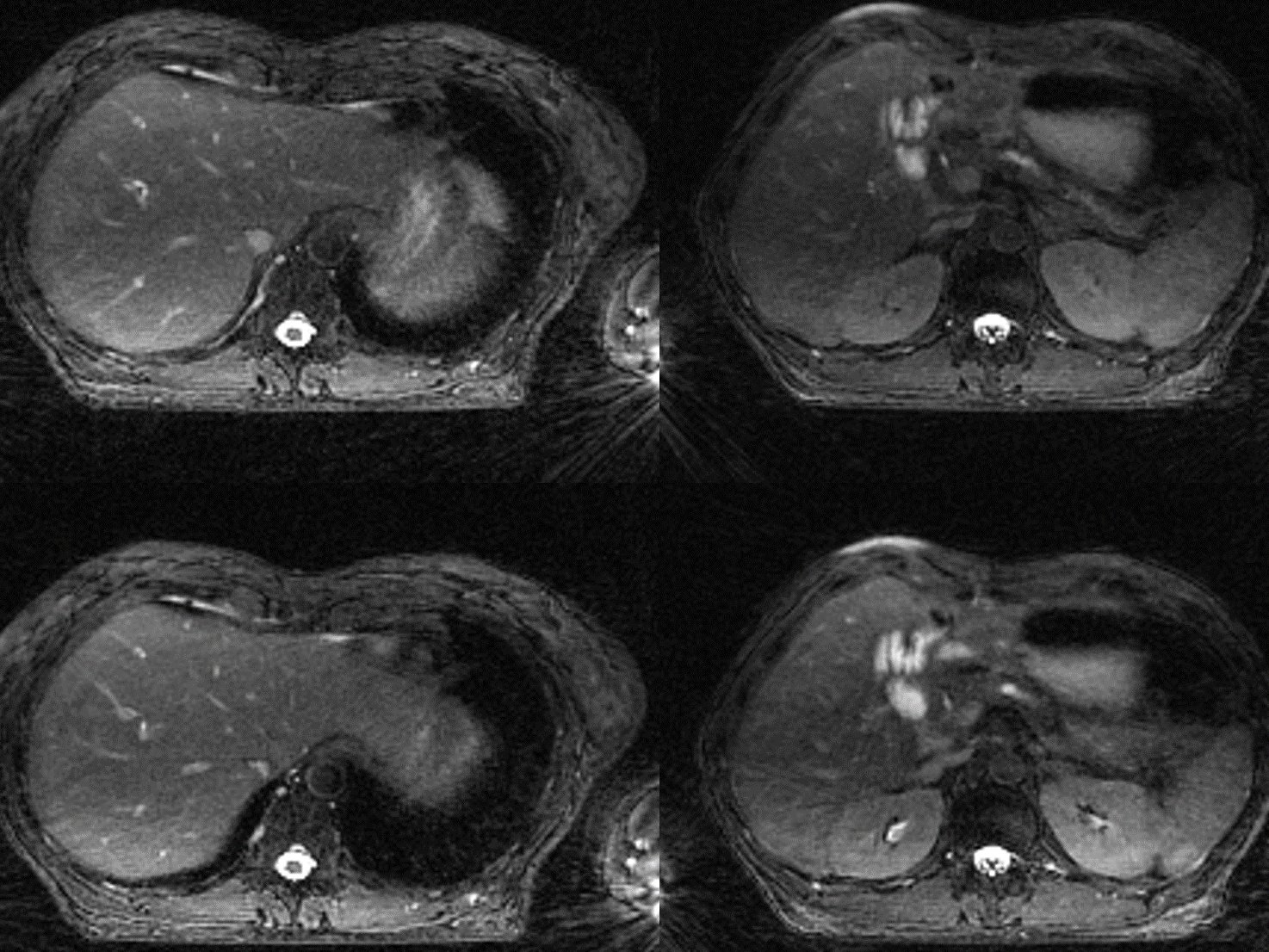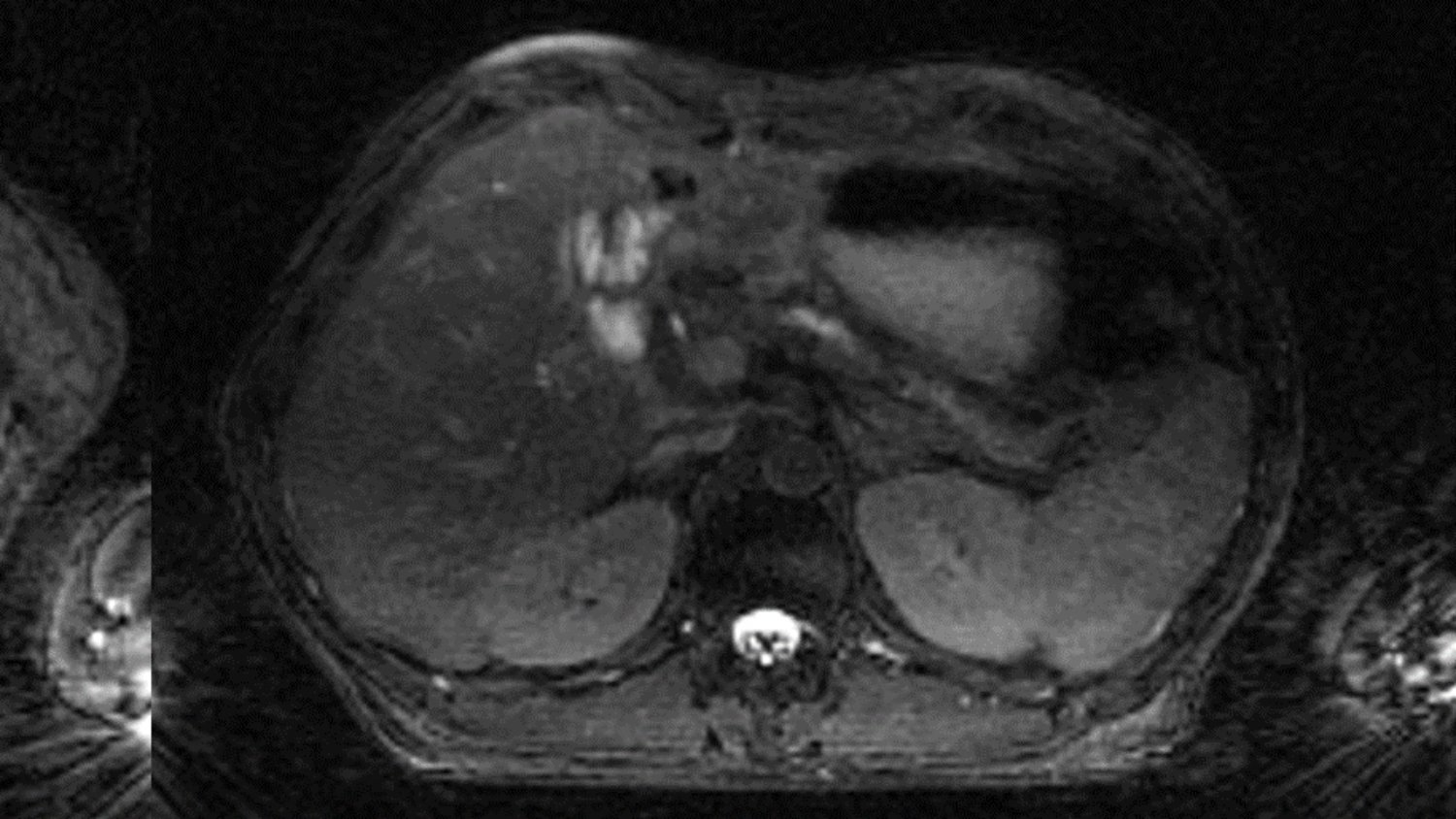
Image: Pancreatic adenocarcinoma 4D-MRI reconstructed using the new high-performance computing method.
Researchers have used methods from high-performance computing to significantly reduce the time it takes to reconstruct images acquired through four-dimensional magnetic resonance imaging (4D-MRI), a leading-edge, high-quality imaging technique.
The reduced reconstruction time may allow clinicians to use 4D-MRI to guide radiotherapy in real time for cancers in the thoracic and abdominal areas. These include liver, kidney and pancreatic cancers, which have proven difficult to treat with radiation because of the proximity of the tumours to vital organs.
The extra precision and accuracy afforded by 4D-MRI guidance makes radiotherapy more effective while minimising side effects. It also provides the opportunity for real-time adaptive radiotherapy, which could revolutionise cancer treatment.
Overcoming the primary obstacle
The barrier to real-time adaptive treatment – known as the online approach – has been the length of time it takes to reconstruct the images from the data acquired during the 4D-MRI scan. Before this research, the reconstruction process took about 17 minutes.
The researchers, who were led by scientists at The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust, set themselves the aim of reducing image reconstruction to below two minutes. This quick turnaround is necessary because the longer the time between scan and treatment, the more likely it is that anatomical changes will have occurred.
For example, when the patient lies on their back, their organs will typically sink towards the back of their body, and their muscles may relax. Any resulting changes in organ position and how the patient breathes will affect the safety and efficacy of the treatment. Also, the procedure is not comfortable for patients, particularly when abdominal compression is used to minimise internal motion.
The researchers managed to surpass their goal, achieving image reconstruction times of just one minute. The study, which was funded by the Cancer Research UK Convergence Science Centre at the ICR and Imperial College London, has been published in the journal Physics and Imaging in Radiation Oncology.
Working with programming experts to find a solution
The research team included experts from the Department of Computing at Imperial, who helped with applying a known algorithm – a set of commands that a computer follows to make calculations – to data from four people with pancreatic cancer.
The data came from the MR Linac Unit based at the Sutton site of the ICR and The Royal Marsden NHS Foundation Trust. This ground-breaking machine can simultaneously perform MRI scans and deliver radiotherapy to patients.
The researchers demonstrated that while using a computer processing unit to run the algorithm reduced the image reconstruction process to less than two minutes, the quickest results were achieved by using a graphics processing unit, which was able to produce images in just 60 seconds.
The researchers also trialled four different data preparation strategies to see how they affected the quality of the images. All of the reconstructed images were deemed identical to the reference ones, achieving a structural similarity index score of above 0.99, where 1 indicates an exact match.
MRI’s increasing role in radiotherapy
In the past few years, adaptive radiotherapy has emerged as a way to enhance personalised care. This approach considers changes to both the tumour and its surroundings in the patient’s body. If the tumour has shrunk slightly since the last treatment or the patient has lost weight, for example, the next radiation dose might be amended accordingly.
Clinicians have increasingly been using MRI in place of computed tomography (CT) in adaptive radiotherapy because it is better at distinguishing between healthy and cancerous tissues. 4D-MRI is more informative than the standard 3D-MRI as it accounts for internal bodily motions, which are dominated by movements related to breathing.
One way to prevent these movements from affecting treatment is to ask the patient to hold their breath, but not everyone can do this for long enough. Abdominal compression belts help reduce the respiratory motion, but in some patients, the organs still move slowly after the belt has been applied.
Respiratory-correlated 4D-MRI could be used to identify phases during the patient’s breathing cycle during which radiation can more easily be delivered to the tumour. This increases accuracy, limiting the damage to the tissue around the tumour. Clinicians use this approach to target tumours that either move with a patient’s breathing or are very close to radiosensitive tissue.
Until now, it has only been possible to take an offline approach. This means that data are captured from the scan and analysed afterwards so that the necessary calculations can be made ahead of the next treatment.
Achieving the best results would require an online approach whereby the 4D-MRI images are reconstructed directly on the scanner. This would allow clinicians to use this real-time information to automatically track the tumour with the treatment beam using a tool called a multi-leaf collimator. As the study has demonstrated, by using a computerised method of reconstructing images, this may now become possible.
Sharing the findings to help more patients
The researchers plan to publish the source code for their fast image reconstruction technique so that others can use it. They are keen to help facilitate its adoption in the hope that it will lead to more patients being treated effectively and safely using respiration-correlated 4D-MRI for online adaptive MRI-guided radiotherapy.
First author Bastien Lecoeur, a PhD student in the Magnetic Resonance Imaging in Radiotherapy Group at the ICR, said:
“We are pleased to have made 4D-MRI a viable option for monitoring internal motions in MRI-guided radiotherapy. The superior soft-tissue contrast that it provides could increase certainty around tumour positions and enable safer, more effective treatments. We hope that this will go on to benefit patients with a range of cancers.”
Dr Andreas Wetscherek, who leads the Magnetic Resonance Imaging in Radiotherapy Group at the ICR, said:
“My team’s mission is to create better MRI-guided radiotherapy workflows so that we can improve treatment for as many people as possible, including those with lung, liver and pancreatic cancer. We hope that this work will open new doors for those with access to an MR Linac system.”
Scientists at the ICR, who have long been at the forefront of radiotherapy research, worked with The Royal Marsden to open the UK’s first MR Linac unit in 2017. Since then, other units have opened, giving more researchers the opportunity to work on optimising radiotherapy workflows in clinical practice.
Looking to the future, Dr Wetscherek believes that we can develop 4D radiotherapy even further:
“Ideally, we will find a way to use time-resolved 4D-MRI, which will provide a volumetric visualisation of the patient’s anatomy for each second of the treatment in real time. If we can get there, we can work the treatment around any type of motion. This would remove the need for patient positioning devices or, in the case of paediatric patients, sedation.”