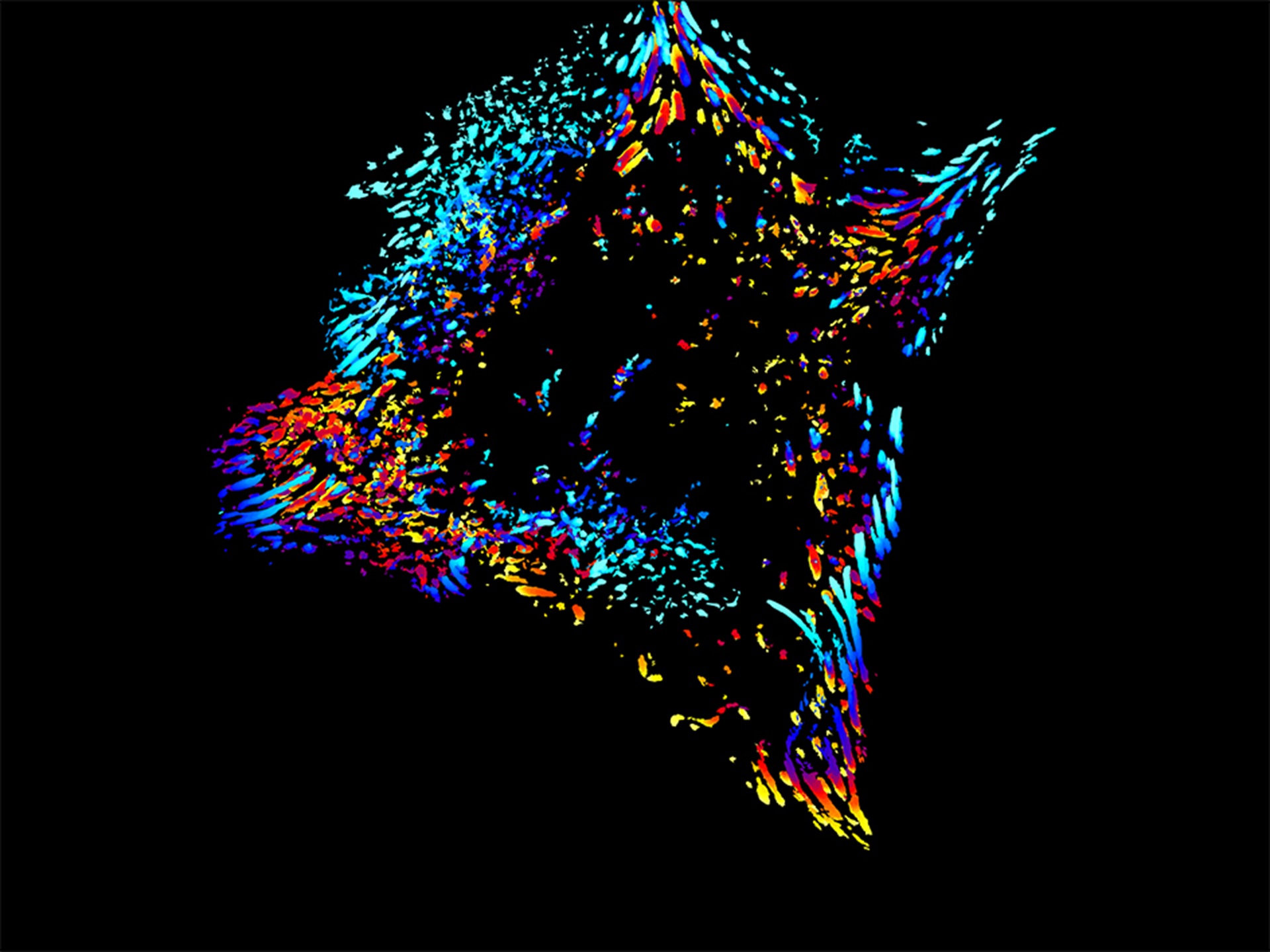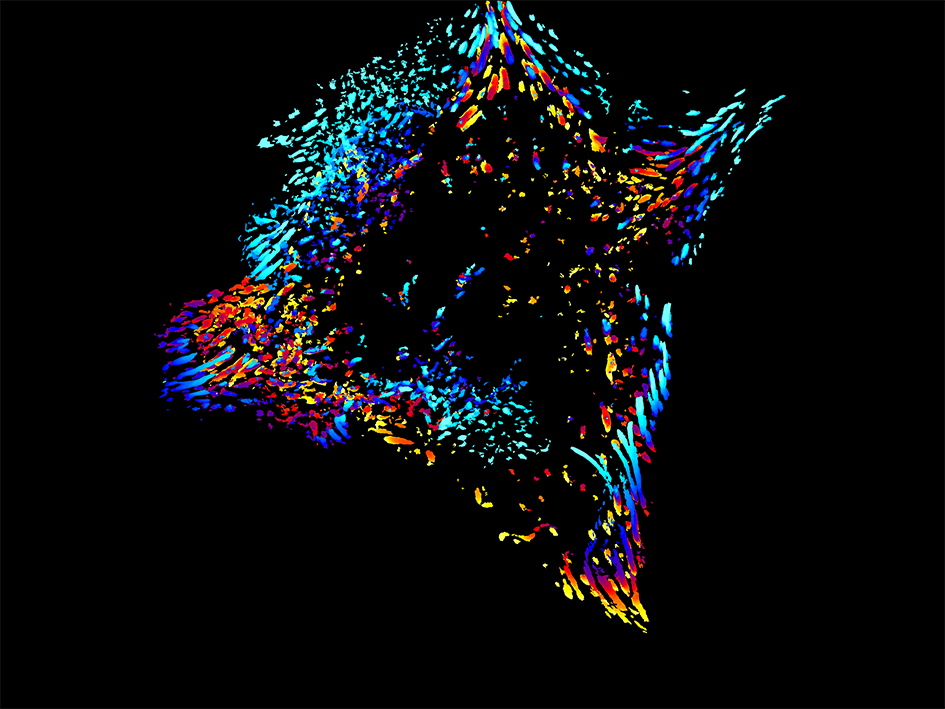
Image: A time lapse image of an aggressive breast cancer cell. Credit: Patricia Pascual Vargas
Scientists have pinpointed thousands of genetic changes in a gene that may increase a person’s risk of developing breast and ovarian cancer, paving the way for better risk assessment and more personalised care.
Researchers from the Wellcome Sanger Institute and their collaborators focused on the ‘cancer protection’ gene RAD51C, finding over 3,000 harmful genetic changes that could potentially disrupt its function and increase cancer risk. These findings were confirmed by analysing data from large-scale health databases.
The findings, published in the journal Cell, are freely available so that they can be immediately used to help doctors better assess cancer risk, especially for individuals with a family history of these cancers, reducing the uncertainty that often accompanies genetic testing.
The study also identified regions of the protein essential for its function, pointing to new roles in cancer development and potential therapeutic targets.
Breast cancer is the most common cancer in the UK, with around 56,800 new cases every year. One in seven UK females will be diagnosed with breast cancer in their lifetime1. Ovarian cancer is the sixth most common cancer in females in the UK, with around 7,500 new cases every year.
RAD51C: a previously unknown variant
The RAD51C gene encodes a protein crucial for DNA repair. Variants in this gene that stop the protein from working are known to increase the risk of breast and ovarian cancers and, in rare cases, may result in Fanconi Anaemia, a severe genetic disorder. Women with a faulty RAD51C gene face a 15 to 30 per cent lifetime risk of developing breast cancer and a 10 to 15 per cent risk of developing ovarian cancer4.
While genetic testing is common for individuals with a strong family history of cancer, the health impacts of most RAD51C variants were previously unknown. This uncertainty over cancer risk often leaves patients and doctors struggling to determine appropriate medical care moving forward.
In this new study, researchers from the Wellcome Sanger Institute and their collaborators including scientists from the Institute of Cancer Research, London, set out to understand the effect of 9,188 unique changes in the RAD51C gene by artificially altering the genetic code of human cells grown in a dish, in a process known as ‘saturation genome editing’.
They identified 3,094 of these variants that may disrupt the gene's function and increase cancer risk, with an accuracy above 99.9 per cent when compared to clinical data. Analysis of UK Biobank data and an ovarian cancer cohort of over 8,000 individuals further confirmed the link between these harmful RAD51C variants and cancer diagnoses.
Mapping the protein structure
By mapping the protein structure, the team also identified crucial surface areas of RAD51C essential for its DNA repair function. These regions may interact with other, yet-to-be-identified proteins or play a role in processes such as phosphorylation, offering valuable insights for drug development and potential new treatment targets.
The study also revealed the existence of ‘hypomorphic alleles’ – a type of variant that reduces the RAD51C gene's function without completely disabling it. These appear to be more common than previously thought and may significantly contribute to breast and ovarian cancer risk.
'This research helps to reduce the uncertainty that can accompany genetic test results'
Rebeca Olvera-León, first author of the study at the Wellcome Sanger Institute, said: “This research demonstrates that genetic risk for breast and ovarian cancer isn't a simple yes-or-no scenario, but exists on a spectrum based on how genetic changes affect protein function. With a more comprehensive understanding of how RAD51C genetic variants contribute to cancer risk, this opens up new possibilities for more accurate risk prediction, prevention strategies, and potentially targeted therapies.”
Professor Clare Turnbull, clinical lead of the study, Professor of Translational Cancer Genetics at The Institute of Cancer Research, London, and Consultant in Clinical Cancer Genetics at The Royal Marsden NHS Foundation, said: “This research helps to reduce the uncertainty that can accompany genetic test results, aiding decisions on monitoring, preventive surgery, or treatment. Given the elevated risks for breast and ovarian cancer, individuals with a harmful RAD51C variant may need to undergo earlier and more frequent cancer screenings.”