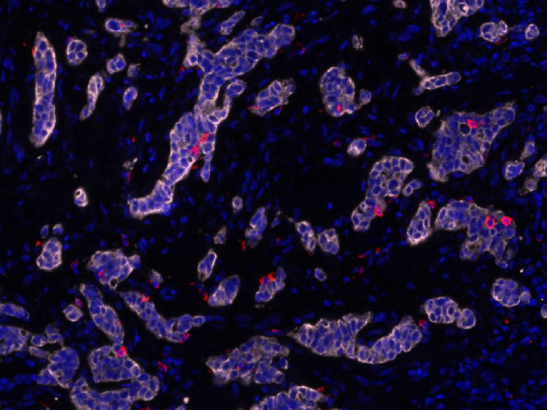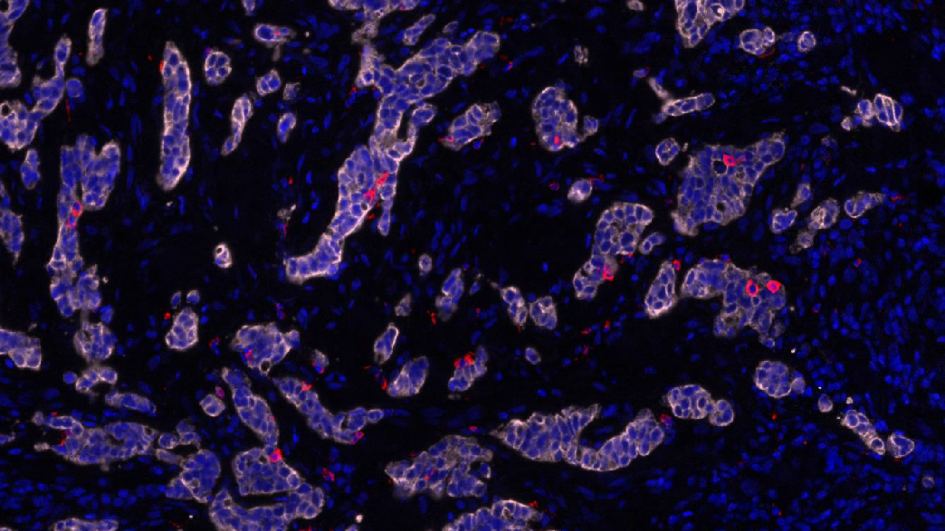
Image: Stomach cancer cells. Credit: Katharina von Loga
A simple and inexpensive blood test could pick out patients with stomach or oesophageal cancer who are likely to benefit from targeted treatment, a new study shows.
The test, known as a ‘liquid biopsy’, detects cancer DNA in the bloodstream to reveal if stomach and oesophageal cancers are being driven by the presence of too many copies of a gene known as EGFR.
Researchers think the test, which is less painful than more invasive tissue biopsies, could be used to identify patients who might benefit from drugs that block EGFR activity, such as panitumumab.
The research team, at The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust, also showed that EGFR inhibitors should never be combined with the chemotherapy drug epirubicin as their effects seem to cancel each other out.
The findings explain why previous trials combining these drugs failed and have major implications for the design of future trials in gastro-oesophageal and other cancers, such as breast cancer, where these two drug types are being tested.
The study is published in the journal Gut and was funded by The Institute of Cancer Research (ICR) – a charity and research institute – as well as Cancer Research UK, the European Union and the NIHR Biomedical Research Centre at The Royal Marsden and the ICR.
Liquid biopsies are a simpler, more convenient option
The team at the ICR and The Royal Marsden looked at the number of EGFR gene copies in tissue and liquid biopsies from patients with advanced stomach and oesophageal cancer enrolled in the REAL3 phase III clinical trial.
The researchers found that abnormally high numbers of copies of the EGFR gene could be reliably detected in tissue and liquid biopsies, which were in agreement 95 per cent of the time.
They concluded that liquid biopsies could therefore be used in place of tissue biopsies in future trials and in the clinic as a simpler and more convenient screening tool to pick out those likely to benefit from EGFR inhibitors like panitumumab.
When the EGFR protein is found at high levels in cancer cells, it causes them to grow and divide – making the disease more aggressive. Drugs that block EGFR work by binding to certain parts of the EGFR protein to slow down or stop cell growth.
Advanced stomach and oesophageal cancers are usually treated with a combination of chemotherapy drugs including epirubicin. When the REAL3 trial was launched in 2009, it sought to find out if adding in the EGFR inhibitor drug panitumumab was better than having chemotherapy on its own.
When the team looked at the first results from the trial back in 2013, they found that adding panitumumab to chemotherapy wasn’t helpful and decided to close the trial early.
Major implications for the design of future trials
When scientists, for this new study, looked at samples from the REAL3 trial, focusing on those patients with abnormally high levels of EGFR, they unexpectedly found that 78 per cent of patients responded to chemotherapy on its own – but only 50 per cent of patients responded to the panitumumab and chemotherapy combination.
The researchers then grew ‘mini-tumours’ in the lab – miniature replicas of patients’ tumours – to explore the reason for the clinical trial findings. They found that the anti-EGFR drugs, when given to a tumour which is also being treated with epirubicin chemotherapy, cause the cancer cells to divide faster and increase tumour growth.
The study findings demonstrate that the new blood test could be used to pick out patients who are likely to benefit from EGFR inhibitors on their own, and also explain why trials like REAL3 that combined EGFR inhibitors with chemotherapy failed.
'Much faster, cheaper and more comfortable for patients'
Study co-leader Professor Nicola Valeri, Professor of Gastrointestinal Oncology at the ICR and Consultant Medical Oncologist at The Royal Marsden, said:
“We have shown that a blood test can pick out just as well as a tissue biopsy cancer patients whose tumours are likely to respond to an important family of targeted drugs. That’s important because it is much faster, cheaper and more comfortable for patients to assess them with a blood test than taking a biopsy.
“Our study also showed that it is important to avoid a combination of targeted drugs and chemotherapy that we had originally hoped would be beneficial. Instead, we think some patients with many copies of the EGFR gene will benefit from just having targeted drug treatment, which we hope will allow them to live longer and with a better quality of life.”
Study co-leader Professor David Cunningham, Director of Clinical Research at The Royal Marsden and Director of the NIHR Biomedical Research Centre at The Royal Marsden and the ICR, said:
“The potential to replace tissue biopsies with a liquid biopsy in some cancers and for some patients could transform our approach to cancer treatment. These results underline the importance of using translational biology to interrogate the results of clinical trials which can be used to determine why treatments fail or succeed.”
The value of liquid biopsies and the potential of 'mini-tumours'
Professor Paul Workman, Chief Executive at the ICR said:
“This promising study is a valuable step towards a more personalised approach to treating stomach and oesophageal cancers. Liquid biopsies are a much better option for patients, as they are a faster and kinder alternative to traditional tissue biopsies.
“This research demonstrates the value of liquid biopsies for guiding treatment and showcases the potential of ‘mini-tumours’, which can shed important insights into the complex biology of cancers and drug interactions.”
Zorana Maravic, Director of Operations at Digestive Cancers Europe (DiCE), a European umbrella organisation representing a large group of patients with digestive cancer, said:
“The results of this study are very important and exciting for the gastric and oesophageal cancer patient community. This is because they have demonstrated that a simple, non-invasive, inexpensive and faster test could identify which patients are likely to benefit from targeted treatment.
“Both oesophageal and gastric cancer, and other digestive cancers, are under-researched and represent an area of high unmet need. Digestive Cancers Europe congratulates The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation on this important work that highlights the importance of collaborative work – between researchers, patients and other stakeholders - towards improving the lives of patients.”