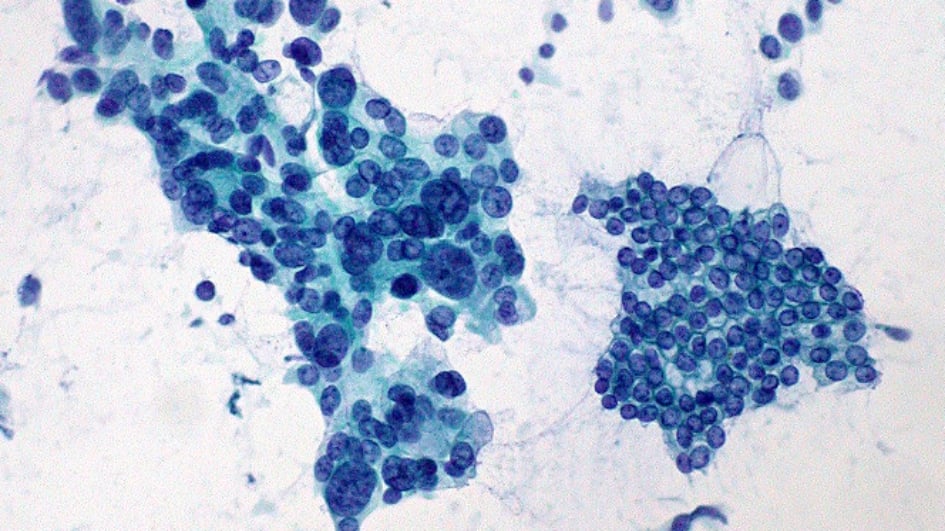
Image: Adenocarcinoma of the pancreas. Credit: Ed Uthman
Pancreatic cancer is notorious for being highly aggressive and difficult to treat. Only one patient in four in England survives more than one year from diagnosis and just seven per cent are still alive after five years. Survival rates for this disease have barely improved at all in the last three decades.
More than 90 per cent of cases of pancreatic cancer are pancreatic ductal adenocarcinoma – a disease that starts in the exocrine cells of the pancreas where digestive enzymes are produced. Pancreatic tumours can often grow and spread unnoticed by the immune system and cause few symptoms, so that by the time they are diagnosed it may be too late to treat the disease effectively.

Image: Roy and his daughters
But now our scientists are beginning to make progress in finding new, more personalised approaches to treating pancreatic cancer. This will offer some hope of a longer and better quality of life for patients and their families – people like Roy Bowdery, who was diagnosed with pancreatic ductal adenocarcinoma in 2014.
Roy recollects: “When I got the diagnosis, my wife and I burst into tears. Pancreatic cancer is the most fatal of all common cancers – it’s really brutal. I’ve been cancer-free for six years, and now my aim is to get into the five per cent who survive 10 years. The figures haven't really improved in the last 40 years. There needs to be research, so more people will survive and get a chance at life.”
Philanthropy plays a key role in pushing forward our vital research into cancers of unmet need, like pancreatic cancer. Donate today to help us make a difference to patients' lives.
Support our work
Understanding the immune landscape
 To improve the odds against this disease, we are using computational analysis of pancreatic cancers to find ways to select patients for more effective, personalised therapies. Dr Anguraj Sadanandam, Team Leader in Systems and Precision Cancer Medicine, is combining use of artificial intelligence (AI) with experimental and clinical studies. He aims to shed light on the different subtypes of pancreatic cancer and the best therapies for patients with each one.
To improve the odds against this disease, we are using computational analysis of pancreatic cancers to find ways to select patients for more effective, personalised therapies. Dr Anguraj Sadanandam, Team Leader in Systems and Precision Cancer Medicine, is combining use of artificial intelligence (AI) with experimental and clinical studies. He aims to shed light on the different subtypes of pancreatic cancer and the best therapies for patients with each one.
The team is particularly interested in using AI to select those patients who are most likely to respond to immunotherapy – a breakthrough type of treatment which directs the body’s own immune system against cancer cells. As pancreatic cancer often evades the immune system, many patients do not respond to immunotherapy, but there are some patients who could significantly benefit from it.
Uncovering potential targets

Image: False colour scanning electron micrograph of a cluster of pancreatic cancer cells grown in culture. Credit: Anne Weston, Francis Crick Institute
Dr Sadanandam said: “Unlike other cancers – for example breast cancer, where huge advances have been made using machine learning approaches – no major developments have been made for pancreatic cancer in decades. Computationally, it’s very important to understand the immune landscape of pancreatic cancer, to help us to develop therapeutics and diagnostics that could lead to personalised treatment.”
AI has allowed researchers to analyse hundreds of patient tumour samples at a time and to spot patterns within that data. Last year a global team led by Dr Sadanandam used AI to analyse the immune response in a rare type of pancreatic tumour called pancreatic neuroendocrine cancer. The researchers were able to pinpoint tumours that hijacked the immune system, and uncover potential targets for immunotherapy to prevent tumours from evading the body’s defences.
Dr Sadanandam’s multidisciplinary approach has also included a first-of-its-kind study that classified pancreatic ductal adenocarcinoma tumours into various subtypes and described the different ways each type responds to treatment. This work has in turn spurred the discovery of further tumour groups by other research teams. His team is now validating these findings, with the goal of eventually offering tailored medicine to individual patients.
Taking a personalised, multi-faceted approach will be essential to overcome such a complex and aggressive disease as pancreatic cancer, and to improve prospects for patients like Roy. Dr Sadanandam and his team are helping to lead the way – addressing a cancer where patients’ needs have been unmet for too long.
This feature originally appeared in Search magazine. Read past issues or subscribe to our supporter newsletter Search.

 .
.