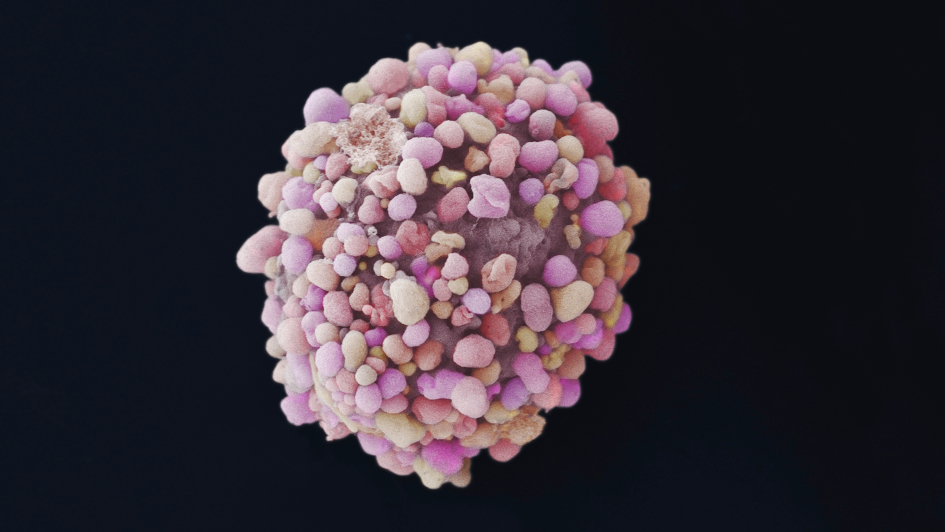
Image: Breast cancer cell. Credit: Anne Weston, Francis Crick Institute, CC BY-NC 4.0
An already approved breast cancer drug could bring hope to thousands of UK women who have an aggressive form of breast cancer, new research has found.
The study, published in the journal Cancer Research, provides a strong case for a clinical trial to test the value of the drug palbociclib in a specific type of triple negative breast cancer.
Breast Cancer Now-funded researchers at The Institute of Cancer Research, London, identified a defect in some triple negative breast cancers that is linked to poorer outcomes for patients and a drug that targets the consequence of this defect.
Much needed treatment
The study suggests that the drug palbociclib, which is currently used to treat other breast cancers that have spread to a different part of the body, has the potential to also be used to treat about a fifth of people living with triple negative breast cancer.
This discovery could provide a much-needed targeted treatment for women who are more likely to see their cancer spread sooner, becoming incurable and often resistant to traditional chemotherapy.
Triple negative breast cancer refers to a diverse group of breast cancers that lack the three molecules which are normally used to classify the disease: the oestrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2).
While these molecules have successfully been used to develop a variety of targeted treatments for other types of breast cancer, the absence of these molecules in triple negative breast cancer means there is a lack of variety in treatment options for this group of breast cancers and as a result triple negative breast cancer is usually treated with a combination of surgery, chemotherapy, and radiotherapy.
Around 55,000 women are diagnosed with breast cancer in the UK every year, and around one in five of these (over 8,000 cases a year in the UK) will be triple negative. This type of breast cancer tends to be more aggressive and disproportionately affects younger women and black women.
This new research, led by Dr Rachael Natrajan, at the Breast Cancer Now Toby Robins Research Centre at The Institute of Cancer Research (ICR) has discovered a way to identify triple negative breast tumours that could be more likely to respond to a class of drugs called CDK4/6 inhibitors, including palbociclib.
'Mini-tumours' to mimic growth in the body
The team screened 200 of the most frequently altered genes in breast cancer to investigate how changes in these genes affect cancer’s ability to grow. Using ‘mini-tumours’ grown in the lab that mimic the tumour growth in a human body, researchers found that triple negative breast cancer cells with alterations that caused a decrease in the levels of a protein called CREBBP, could grow faster and more aggressively.
The team then used two large patient databases to further investigate what happens when CREBBP levels in the tumour are low, and found this to be linked to poorer survival rates for patients with triple negative breast cancer. Furthermore, low levels of this protein occur in a variety of other cancers including uterine, ovarian, and some lung and bladder cancers, suggesting it plays a vital role in tumour development or growth.
Understanding what drives growth in specific tumours
They found that when CREBBP levels are low, tumour cells switch to a different way of multiplying relying on proteins called CDK4 and CDK6. These proteins can be blocked with a group of drugs known as CDK4/6 inhibitors, which stops the cancer from growing.
Palbociclib is a CDK4/6 inhibitor that is currently used in the UK to treat some secondary (or metastatic) breast cancers. The researchers tested the effectiveness of palbociclib on cancer cells with CREBBP alterations in the lab and in mice.
The drug was effective even when tested on standard chemotherapy-resistant triple negative breast cancer cells, that lacked CREBBP, donated by a patient.
Overall, this study shows that palbociclib successfully stops the growth of triple negative cancer cells when they have low CREBBP levels, suggesting that this could be a successful new treatment for this type of breast cancer.
While not all triple negative breast cancer tumours have low CREBBP levels, it is the case in about a fifth of patients. This means that measuring CREBBP protein levels in tumours could help to identify thousands of patients that could benefit from a treatment that is already approved for use in the UK.
A strong case for a clinical trial
Being an already licenced drug, already proven to be safe, means palbociclib can be quickly progressed into clinical trials for triple negative breast cancer and potentially benefit patients sooner. This study provides a strong case for a clinical trial into the use of palbociclib for triple negative breast cancer tumours with low CREBBP levels.
Dr Rachael Natrajan, Team Leader in Functional Genomics at The Institute of Cancer Research, London, said:
“Our study shows what drives the growth of some triple negative breast cancers and suggests the exciting possibility that an already-approved breast cancer drug could be used to help women with this type of disease.
“Our findings were only possible because we used an innovative model, involving the growth of 3D ‘mini tumours’ in the lab, to more closely reflect how tumours develop in the body.”
'Hugely exciting'
Dr Simon Vincent, Director of Research, Support and Influencing at Breast Cancer Now, said:
“It’s hugely exciting that this research has uncovered a new possible use for palbociclib as a targeted treatment for some women living with triple negative breast cancer.
“Each year, around 8,000 UK women are diagnosed with this aggressive form of breast cancer and we desperately need new, effective ways to treat them and stop them dying from this devastating disease. We hope that if clinical trials confirm that palbociclib is beneficial for some of these women, it will be advanced through the approval process and made available for those who need it as quickly as possible."

 .
.