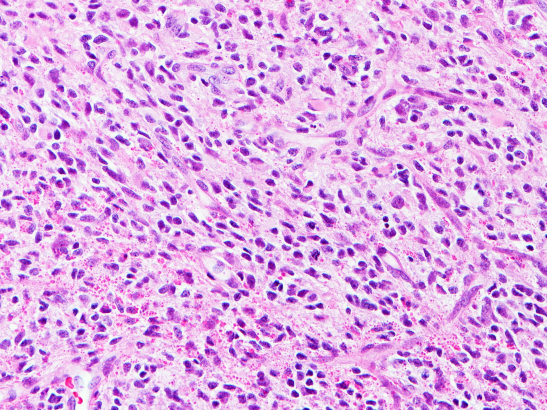
Image: A type of glioma. Credit: David Ellison, St. Jude Children’s Research Hospital
Ribociclib – a drug already used to treat breast cancer – may help slow the growth of diffuse hemispheric glioma (DHG), new research has found.
In research published in the journal Cancer Cell, a team of scientists from The Institute of Cancer Research, London and the Dana-Farber Cancer Institute, Boston, USA, uncovered clues about the growth of a specific type of DHG – DHG, H3G34-mutant – which allowed them to explore new targeted treatments. The research was partly funded by The Brain Tumour Charity and Cancer Research UK.
Tumour cells disrupt development of neurons
Diffuse hemispheric glioma is a rare, high-grade childhood brain tumour with a prognosis of 18-22 months; there is currently no cure. It is estimated that more than 30% of all paediatric high-grade glioma diagnoses are the DHG-H3G34 variant.
Laboratory tests and pre-clinical models led the researchers to discover that tumour cells disrupt the normal development of neurons, causing them to look like immature early neuron-like cells.
Searching for novel treatments
Exploring what would make these cells vulnerable to novel treatments found that targeting the protein CDK6, which is involved in regulating cell division, could prove promising. Abnormal activity in the CDK6 protein can lead to uncontrolled cell division – a hallmark of cancer.
Ribociclib is a CDK4/6 inhibitor approved to treat breast cancer, but in this study, it was used to treat a child with a brain tumour when other treatments failed. Treatment resulted in stable disease for a further 17 months until it started to grow back.
These very early results are remarkable given the typically poor prognosis for children diagnosed with these aggressive brain tumours.
The child is currently undergoing further treatment, more than four years since her diagnosis.
Clinical trials on the horizon
While ribociclib is not a cure for this devastating brain tumour, these findings are significant because the disease typically progresses within 3.5 months following recurrence.
There are hopes that this research could pave the way for clinical trials, as this was a preliminary test in just one child.
This research also showed that DHG-H3G34 tumours are more responsive to CDK4/CDK6 inhibitors than other high-grade glioma types – opening the door for more targeted treatments for this genetically distinct tumour type.
CDK4/6 inhibitors could be used in a combination treatment strategy
As CDK4/6 inhibitors slow the grow of tumour cells and do not kill them, this would not be a standalone treatment and therefore combination therapies need to be explored.
Professor Chris Jones, Professor of Childhood Brain Tumour Biology at The Institute of Cancer Research, London, said:
“This work shows the importance of understanding how brain tumours develop in order to figure out better ways to treat these patients.
“It was a surprise to realise that this type of glioma seemed to arise from developing neurons, but we were able to use this knowledge to find specific vulnerabilities in these cancer cells, which hopefully we can now translate into clinical trials.”
'Thrilled to see our work translate into helping a patient so quickly'
Mariella G. Filbin, MD, PhD, Co-Director of the Paediatric Neuro-Oncology Program at Dana-Farber Cancer Institute, said:
"Our trans-Atlantic collaboration helped tremendously in validating and expanding our results, and I am thrilled to see our work translate into helping a patient so quickly. This is the first time we found functional consequences of aberrant lineage specification in tumour cells—a result that was unexpected at first, but is now setting the stage for new therapeutic avenues in this disease.”
Dr Simon Newman, Chief Scientific Officer at The Brain Tumour Charity said: “This research helps us have a better understanding of what is driving this devastating disease in children.
“We know that current treatments are not effective and that finding vulnerabilities in cancer cells could lead to new targeted treatments to help children live longer and better lives. Although this is very early days, we hope that it will provide some data to inform clinical trials in the future.”
Personal Story: Billie Bainbridge
The Research was in part funded by The Billie Butterfly Fund in memory of five-year-old Billie Bainbridge who was diagnosed with an incurable brain tumour in June 2011.
The Bainbridge family, from Exeter in Devon set up the fund to raise money for treatment of Billie’s diffuse midline glioma – an aggressive childhood brain tumour.
Treatment options for these aggressive brain tumours are currently limited to radiotherapy but this is considered palliative. Billie received radiotherapy in London which shrank her tumour, followed by steroids, after which her treatment team said no more could be done.
When she was diagnosed, Billie’s family were told her prognosis was less then 12 months, and despite travelling to the Houston, Texas for a clinical trial to extend her life, Billie died at home less than a year after her diagnosis.
Now, twelve years on, the money raised for the Billie Butterfly Fund has contributed to this, and other research that could pave the way for future treatments for children diagnosed with aggressive brain tumours.
Since Billie’s death the family have been touched by more tragedy as her mum Terri died from aggressive breast cancer that was diagnosed before Billie’s brain tumour, and her grandad, Peter Bainbridge, who visited Professor Chris Jones’ laboratory with her dad Sam has also since died.
Sam Bainbridge, Billie’s dad said: “We had phenomenal support from friends and family to raise a huge amount of money to help Billie, the money left was donated to The Brain Tumour Charity to fund this important paediatric research.
“We are so amazed to hear that the research has led to positive developments, and while we understand this is not yet the cure we so desperately need, the potential to help children live longer feels like a huge step forward.
“It’s impossible to describe how desperate and helpless you feel when you’re told your child has months to live, and there’s nothing that can change that. I hope that this research and future research will give hope to families who are now sadly experiencing the horrific circumstances we all endured.
“Billie was the brightest, most beautiful girl. Loved by everyone she met. She coped amazingly with her condition, and everything she went through. She is sorely missed every day.”

 .
.
 .
.