
Roulette wheel image from pixabay.com. CC0 Public Domain
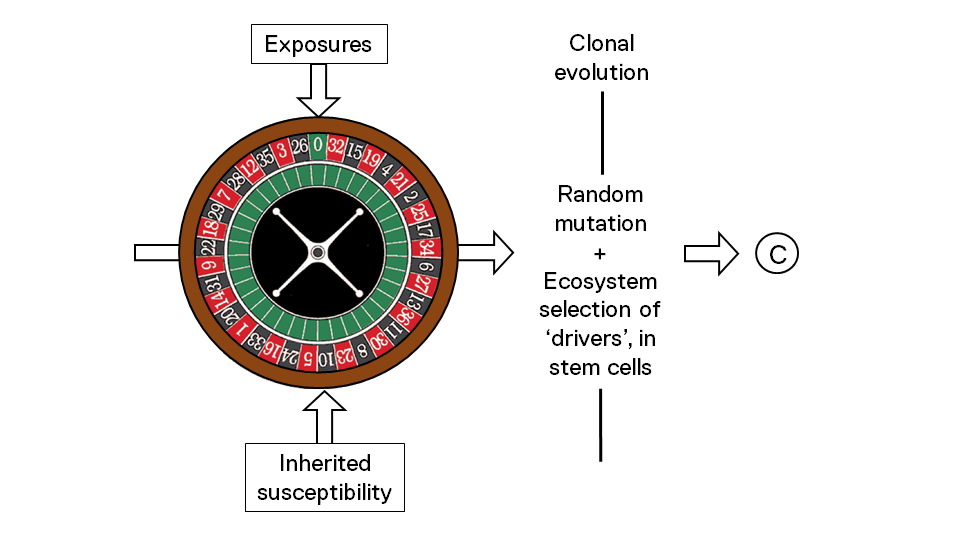
In January of 2015, Christian Tomasetti and Bert Vogelstein from Johns Hopkins Hospital in the U.S. set the cat among the pigeons by suggesting that some two thirds of human cancers were down to chance alone – in other words through random mutations in dividing stem cells, with no influence of either background genetics or exposures. The depressing message is that we can do nothing about most cancers. It’s just bad luck.
Their paper prompted a barrage of letters to Science, as well as editorials and blogs, pointing out deficiencies in their data and arguments. I think Tomasetti and Vogelstein are both right and wrong.
They are right in so far as each round of DNA replication in a stem cell – the primary target for cancerous transformation – will impart a risk.
This risk derives from unrepaired or misrepaired errors in copying and editing, or from internally inflicted DNA damage, say from our oxidative metabolism.
Mutations that register in stem cells and increases their fitness – by allowing them to divide more rapidly, for example – will also carry a risk.
So the invention of immortal stem cells, some 600 million years ago, will have created a malignant liability – although one that has naturally been countered by the co-evolution of adaptive constraints[1].
Still, more stem cell cycles = more intrinsic risk of cancer? Probably.
Tomasetti and Vogelstein provided some evidence that tissues with more replicating stem cells more frequently give rise to cancer of that tissue type, as you might expect to be the case.
Similarly, the different spectrum of cancer types in children versus adults probably reflects timed developmental windows when specialised stem cells are active[2].
But how can it be concluded that random error or chance alone is all it takes for any cancer, let alone most? I suggest it’s a misunderstanding of a fundamental kind.
Several decades ago, Richard Doll and Richard Peto[3] suggested that all cancers are caused by a multi-factorial mix of background genetics, exposures and chance. I see no reason to disagree with them and the evidence suggests they were correct.
To date, genome-wide association studies here at The Institute of Cancer Research, London, and elsewhere have uncovered inherited (or germline) genetic variants that confer increased risk for each and every one of the cancer types evaluated, including all the common adult cancers. So far there are no recorded exceptions. The actual contribution of constitutive genetics to risk is extremely variable, from rather low for lung cancer to high for testicular and prostate cancer. But it’s always there as a causal ingredient.
Worldwide cancer incidence data from registries make it clear that all the major cancers vary in incidence, from 2- to 400-fold, over time and place and in a way that can only be explained by social or lifestyle-associated factors, rather than population genetics.
If there was any cancer cause that could be ascribed to just chance error alone, I would guess that it could be some of the paediatric cancers. Their incidence (e.g. for Wilms tumour) varies very little and they could be regarded as sporadic developmental errors. But for common cancers, Tomasotti and Vogelstein are surely wrong.
But then they are right again, but in a manner for which they can claim little credit.
What set of gene variants we each inherit from our parents is down to the lottery of the genetic shuffling that operates at the moment of conception – along with prior historical accidents in the germline.
What we are exposed to, and when, where and whether it does or does not lead to a ‘driver’ mutation in a relevant cell type, is riddled with chance and circumstance.
Endogenous or exogenous causes of cancer-causing mutations – causes from within the cell or body, or outside them – may leave particular signatures of DNA damage but they are indiscriminate in the effect of that damage on genes.
They are effectively blind marksmen. As in evolution in general, mutational diversity is blind to utility[4].
In cancer therefore, it is pot luck whether cigarette carcinogens strike a gene, and in a manner that results in a potentially cancer-causing fitness advantage for the cell.
But, by and large, the more throws of the dice the more likely it is that a mutation endowing a fitness benefit will emerge. Hence genetic instability – both in bacteria under stressful eco-pressure or cancer cells under genotoxic attack, genome-wide instability is a gamble that can pay off.
‘There is a mystery here – I don’t think even Professor Doll could elucidate it – the mystery of the thousands of people who had smoked like chimneys without coming to any harm.’
(The journalist, Bernard Levin, 1997)
So, here’s a way to look at it: the cause of each and every cancer has a hefty component of chance, or bad luck. It explains the conundrum of why many lifelong smokers get lung cancer, but even more do not. The genetic variants we inherited from our parents are unreturnable goods and many chance events are non-negotiable. Fortunately for us, exposures are major contributors to risk and offer a route to risk reduction or prevention.
The formation of cancers that are potentially preventable through prophylactic treatment (e.g. HPV vaccines), prudent avoidance (e.g. cigarette smoking, sunbathing) or modified diets is difficult to calculate. Epidemiologists have, in the past, suggested 75-90%. In response to the Tomasetti and Vogelstein paper, Cancer Research UK issued a release, based on a 2010 paper by Parkin et al, saying that 42% of cancers in the UK had known avoidable causes. That’s not very different from Tomasetti and Vogelstein’s one third!
The data in the Parkin paper may well be correct but its limitations are important. The study looks at 14 potentially avoidable lifestyle exposures for the risks they contribute to 18 different cancers in the UK. Several cancers are excluded including prostate, brain and non-melanoma skin cancer. Infection contributes an estimated 3% of risk, yet in the less developed parts of the world this might rise to as high as 40%. Breastfeeding is the only listed reproductive risk factor. Calorific intake, exercise and energy balance are not considered under dietary factors. The estimate of risk from individual exposures is confounded by the complex interactions between different factors – for example inherited genetics, reproductive factors and diet in breast cancer.
But for all this complexity, there is a clear clue to the right answer from the documented variation in incidence rates. This suggests to me that up to some 90% of common cancers could, given sufficient knowledge and applied effort, be prevented or avoided. Now I’m dreaming. But I’m probably not alone.
References
- Greaves M (2000)Cancer. The Evolutionary Legacy.Oxford University Press, Oxford.
- Greaves M (2015)Origins and evolution of pediatric cancers.In: Nathan and Oski’s Hematology and Oncology of Infancy and Childhood, eighth edition (eds Orkin SH, Fisher DE, Ginsburg D, Look AT, Lux SE, Nathan DG).Elsevier Saunders, Philadelphia, pp 1229-1238.
- Doll R, Peto R (1981)The causes of cancer.Oxford University Press, Oxford.
- Monod J (1970) Chance and necessity. Alfred A Knopf, New York.