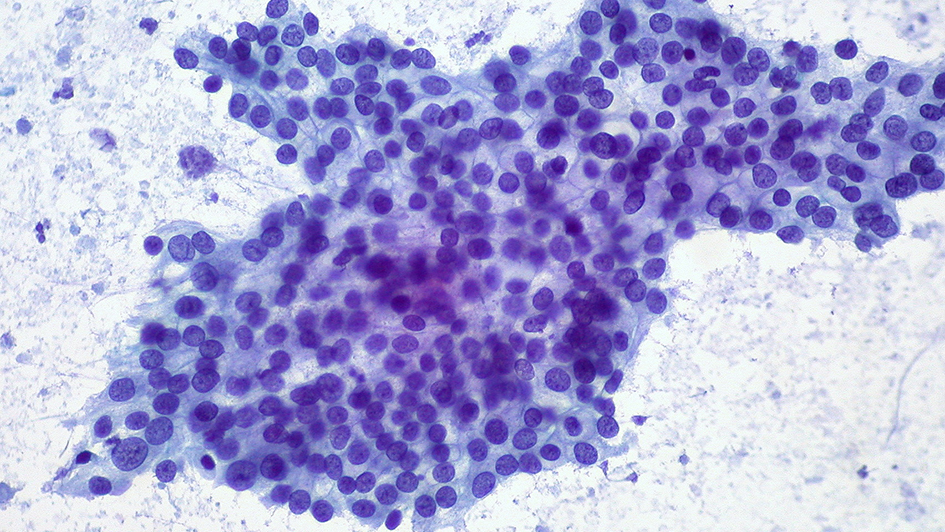
Adenocarcinoma of the pancreas (photo: Ed Uthman/CC-BY-2.0)
In recent years, cancer researchers have understood that tumours are far from a simple collection of fast-growing cells.
In fact, there can be an extraordinary amount of variability between different tumours and within different cells in the same tumour.
This is known as tumour heterogeneity – and understanding how it arises and affects a patient’s cancer is key to establishing truly personalised treatments.
But what drives these differences? Researchers here at The Institute of Cancer Research, London recently published a review in the journal Cancer Research on how tumours change and what factors affect their evolution.
While scientists have focused on the flaws in a cancer cells’ DNA, the local tumour environment, energy use and cell origin can also play a large role in how a tumour develops.
Not just genes drive cancer
One of the key events that can lead to cancer is the accidental mutation of an oncogene. These are genes that can be easily altered from a normal healthy function to a version that drives uncontrolled cell growth.
For example, KRAS is an oncogene often found in many cancers, including 90% of the most common type of pancreatic cancer.
The KRAS protein sits on the surface of a cell and, when activated, tells the cell to grow. But in cancer cells, the KRAS protein can be mutated so that it’s permanently switched on – constantly giving the growth signal.
Uncovering these genes like KRAS and figuring out ways to target them with drugs has been a staple of cancer research for decades.
The ICR’s Dr Anguraj Sadanandam explains that in addition to genetic changes, there are many other processes that affect cancer’s development: “We know that grouping patients by the genetic profile of their cancer has already led to advances in the clinic.
"Our work suggests that profiling cancers by their metabolism or the type of cell that originally started the cancer could have a similar therapeutic benefit.”
A product of their environment
One example of how the environment can affect tumour development is a lack of oxygen. Known as hypoxia, this occurs when blood vessels weaken near the tumour and not enough oxygen reaches the cancer cells.
A bit like an oxygen mask dropping down for an aeroplane passenger when the cabin pressure drops too low, cells in this situation gain ‘emergency access’ to genes that allow the cells to survive.
These genes reduce the cells’ dependency on oxygen in the short term by changing the way they process fuel. They also send chemical signals to call for a new blood supply, or enable the cell to move around the body to seek out the nutrients and oxygen they need.
Either way, the cancer cells have fundamentally changed, not because of changes to the DNA code, but because the genes available to be read have been altered. This process of restructuring DNA to prevent some genes from ever being expressed or allowing other genes to be expressed more often is known as epigenetics.
Together these methods – genetic faults, environmental pressures and epigenetic changes – form a system to influence the development of cancer.
But what does this mean in practice?
Defining pancreatic subtypes
Dr Sadanandam suggests that clinicians should be analysing the proteins being produced by cancer cells as well as the genetic faults in its genome: “Until recently, the majority of cancer research was focused on gene expression because the technology was better for measuring these molecules at that time.
"However, new technologies are becoming available which allow researchers to study tumours in even more detail. It’s not just the faults in cancer’s DNA that’s important but how they alter its expression to suit their needs.”
As an example of this, Dr Sadanandam and colleagues carried out a study, published in Cancer Discovery, which classified pancreatic neuroendocrine tumours in the lab using an array of different techniques.
The researchers looked at the RNA of the cancers cells, which indicates what proteins they are actually producing, as well as mutations in the DNA and energy consumption. As a result they were able to classify the cancers into three main subtypes: ‘insulinoma-like’, ‘metastatic-like” and an intermediate subtype.
The “insulinoma-like” cancers were normally derived from beta-cells in the pancreas, which use sugar to make insulin for the body. Cancers generated from these cells seemed to have a similar approach to producing energy to beta cells, and were much less likely to spread than other subtypes.
‘Metastatic-like primary’ cancer cells, however, made use of proteins that are not normally expressed by beta-cells, and used a very different method for processing energy. These cancer cells probably evolved from stem cells in the pancreas and were far more likely to spread around the body.
Importantly, this breakdown of different subtypes would not have been possible with a purely genetic approach. This more complete analysis could be essential in the future for determining which patients’ tumours are likely to spread and what treatments may be most effective.
Dr Sadanandam and an international team of scientists conducted a similar analysis, published in Nature Medicine, of pancreatic ductal adenocarcinomas – the most common type of pancreatic cancer.
Pancreatic ductal adenocarcinomas were thought to be fairly uniform since they have the same genetic faults – such as the KRAS mutations described earlier.
But upon closer inspection, the way in which these genes were expressed could be markedly different. The ‘classical’ subtype produced much more of the faulty KRAS protein, suggesting that tumour growth was dependent on its signalling, while a subtype known as ‘quasi-mesenchymal’ showed a higher expression of genes that allowed it to be more adaptive.
And these subtypes had very different responses to the two most common therapies for pancreatic cancers. The classical subtype was more responsive to the drug erlotinib, while the ‘quasi-mesenchymal’ cancer lines were susceptible to gemcitabine.
From tumour evolution to treating patients
Genetics, metabolics and molecular changes within the cell all contribute to tumour heterogeneity and the clustering of cancers within different subtypes. By focusing on genetics alone, clinicians might be missing the clues they need to decide on the best treatment for patients.
Initially, some key genetic mutations may start an otherwise healthy cell on the path to becoming a cancer cell. But later, a secondary genetic or metabolic change can drive further progression and affect a patient’s prognosis.
Dr Sadanandam explains: “Research has already shown success in the clinic by designing drugs that target genetic flaws unique to cancer subtypes – such as giving tamoxifen to breast cancer patients that are estrogen receptor positive.
“In the future, designing treatments that take into account a cancer’s environment and metabolism could save yet more lives.”
comments powered by